There are many risk factors that can lead to a stroke. A healthy lifestyle can prevent a stroke in many cases. Learn all the important information in this article.
A stroke can suddenly and drastically change your life. During a stroke, the blood supply to part of the brain is interrupted, and the brain no longer receives sufficient oxygen. Even short periods of oxygen deprivation can lead to the death of nerve cells (neurons). Therefore, a stroke is a serious medical emergency that requires immediate intervention to quickly restore oxygen supply and prevent major brain damage. This means that the faster a stroke patient is treated, the greater the likelihood of avoiding permanent impairments ("Time is Brain").
Fortunately, there are ways to reduce the risk of stroke. Through a combination of a healthy lifestyle, regular medical check-ups, and heightened awareness of risk factors, many strokes can be prevented.
In the following article, we go into detail on how you can prevent a stroke, what risk factors exist, and how to determine if you have had a stroke.
Key Facts
- Types of Stroke: Ischemic (80-85%) and hemorrhagic (15-20%); transient ischemic attack (TIA) is a warning sign for future strokes.
- Prevention: Control blood pressure and cholesterol, maintain a healthy diet, regular exercise, quit smoking, limit alcohol consumption, maintain a healthy weight.
- Symptoms: Sudden vision issues, speech difficulties, paralysis, dizziness, severe headache.
- FAST Test: Face drooping, Arm weakness, Speech difficulties, Time to call emergency services.
- Diagnosis: CT scans detect blood clots or hemorrhages, MRI provides detailed brain imaging.
How Does a Stroke Develop?
A stroke can be caused by a vascular occlusion or a hemorrhage. In both cases, this leads to restricted oxygen supply to the brain, which can result in the death of brain cells. Below, we provide an overview of the different types of stroke:
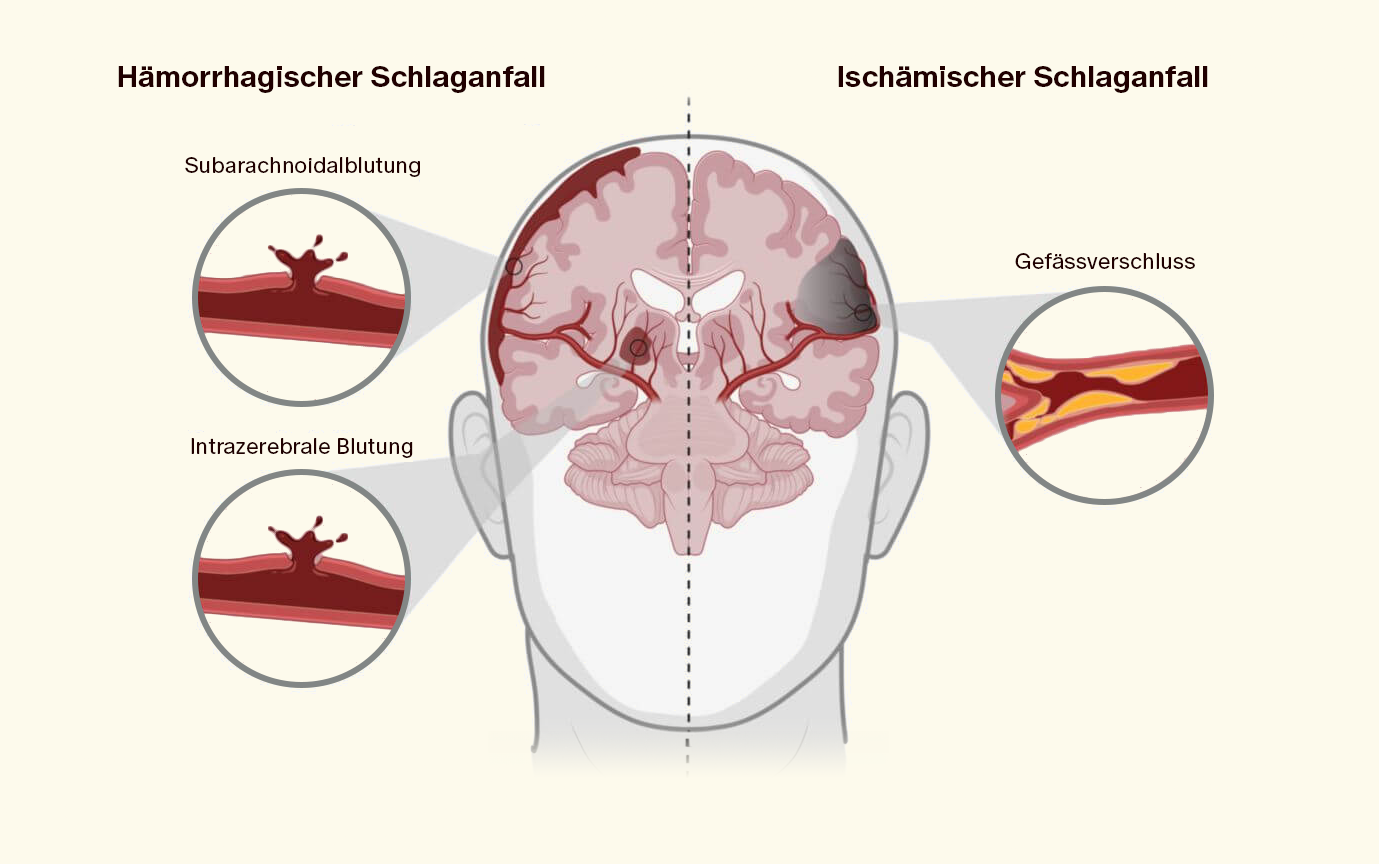
Ischemic Stroke
An ischemic stroke, also known as a brain infarction, accounts for 80 to 85% of all strokes. It refers to a lack of blood flow (ischemia) due to narrowing (stenosis) or occlusions in the arterial supply to the brain:
- Blood clot (Thrombus): A blood clot may form either directly in the brain arteries or can be transported through the bloodstream where it can lodge in a narrowed blood vessel and block the blood flow (embolic stroke).
- Calcium and fat deposits (Plaque): Calcified and fatty deposits in the blood vessel wall (plaque) can narrow the vessel's lumen, blocking blood flow to the brain and triggering a stroke. Moreover, plaques can dislodge and travel through the bloodstream to the brain arteries. When plaques tear, they can form blood clots that lead to a vessel occlusion. Additionally, a team of doctors from LMU Clinic found that one-third of patients with an unexplained cause of stroke had complex plaques in the carotid artery.
Hemorrhagic Stroke
A hemorrhagic stroke ("hemorrhage" means bleeding) is also known as a cerebral bleed resulting from a burst or torn blood vessel. It distinguishes between more common intracerebral hemorrhages (ICH) and less common subarachnoid hemorrhages (SAH). ICH refers to bleeding into the brain tissue; SAH refers to bleedings into the subarachnoid space. About 15-20% of strokes are due to bleeding. Brain hemorrhages can be triggered in various ways, for example by:
- Traumatic brain injury (TBI)
- High blood pressure (hypertension)
- Vascular malformations in the brain
Transient Ischemic Attack (TIA)
A transient ischemic attack (TIA) resembles a stroke in its symptoms and leads to temporary neurological disturbances that usually resolve within 24 hours. It is important to note that there is no uniform definition for a TIA. It is known to be caused by an oxygen deficiency in certain areas of the brain. This deficiency is tolerable for a short period in this context and usually causes no permanent damage.
Although a TIA is not a classic stroke, it can still be a precursor to a future stroke. About 10% of patients with a TIA experience a major stroke within the following 7 days.
How Can I Prevent a Stroke?
- Control of high blood pressure
- Control of cholesterol levels
- Healthy eating
- Regular exercise
- Non-smoking
- Limiting alcohol consumption
- Weight control
Control of High Blood Pressure
High blood pressure is one of the main risk factors for stroke and the main cause of heart diseases. According to statistics, in 2022 approximately 20% of the population in Switzerland were affected by high blood pressure or were taking medication for it.
Fluctuations in blood pressure throughout the day are entirely normal. For example, your blood pressure changes depending on whether you are active, resting, or stressed. The diagnosis of high blood pressure (hypertension) means that your blood pressure is elevated over a long period.
High blood pressure can lead to a stroke in various ways. High blood pressure puts strain on blood vessels throughout the body, including those supplying the brain. If the arteries are under constant pressure due to high blood pressure, changes occur in the vessel walls, and the delicate inner lining (intima) can be damaged. To withstand the high pressure, the vessels thicken and stiffen. This is done by increasing muscle mass and collagen fibers in the vessel wall, which reduces the flexibility of the vessels and narrows their lumen. As a result, a narrowing of the vessels occurs, which can lead to circulatory disorders.
High blood pressure can cause small wounds in the vessel's inner wall, where plaque can form. Plaque consists of fats, cholesterol, calcium, and other substances in the blood that can accumulate on the vessel walls. These deposits clog the blood vessels (arteriosclerosis). As a result, blood flow decreases, and the oxygen supply to the brain and other organs is impaired. Atherosclerotic altered blood vessels are also more susceptible to rupture. If a blood vessel in the brain bursts, this can lead to a hemorrhagic stroke.
Cholesterol Levels & Apolipoprotein B (ApoB)
Cholesterol is vital for our bodies and is essential in the formation of cell membranes and other processes. It's important to know that we do not obtain cholesterol solely through diet (25%) but that our bodies also produce it (75%). However, cholesterol levels should be monitored.
Cholesterol, like fat, is not soluble in water (or blood). Therefore, it needs a connection of proteins, fats (lipids), and other components for transport. These connections are called lipoproteins, including LDL (Low-Density Lipoprotein) and HDL (High-Density Lipoprotein). These lipoproteins can be deposited in the vessel wall and lead to arteriosclerosis.
A study compared the effects of lowering LDL cholesterol to a low level (2.3-2.8 mmol/L or 90-110 mg/dL) with a very low level (under 1.8 mmol/L or 90 mg/dL). It should be emphasized here that these values are not internationally recognized reference ranges and were set by the study leaders beforehand. Thus, they may vary depending on the country or laboratory. The study showed that a very low LDL cholesterol level is better at preventing another stroke. Over a period of 3.5 years, 1 in 9 patients with low LDL cholesterol experienced another stroke or heart attack, compared to 1 in 11 patients with very low LDL cholesterol.
Another study reviewed results from 26 studies involving a total of 170,000 patients. There was a clear link between lowering LDL cholesterol and reducing the risk of stroke. Lowering LDL cholesterol by 1 mmol/L (38 mg/dL) reduced the risk of stroke by an average of 20%.
Although high cholesterol levels are often associated with arteriosclerosis, they alone are not an indicator of potential stroke risk.
Therefore, apolipoprotein B (apoB) should also be measured alongside cholesterol. ApoB measures the number of atherogenic lipoprotein particles in the blood, while cholesterol measures the amount of lipoproteins. A high level of ApoB can indicate that a person has many of these harmful particles in their blood, even if the cholesterol level is within normal limits. Highly published studies have shown that apoB is the main indicator for arteriosclerosis (deposition of cholesterol in the vessel walls).
Another advantage is that cholesterol levels can be influenced by triglycerides, especially in patients with metabolic syndrome. ApoB is less susceptible to these fluctuations and can therefore provide a more reliable measurement of cardiovascular risk. An elevated level of ApoB can indicate a disrupted lipid metabolism, which can be associated with insulin resistance and metabolic syndrome.
But what exactly is the relationship between cholesterol and ApoB? Apolipoproteins surround fatty acids and form a water-soluble shell. In this way, fatty acids can be transported in the blood. Apolipoprotein B is a protein that plays a significant role in lipid metabolism. It is the main component of atherogenic lipoproteins (such as LDL or VLDL), i.e., those lipoproteins involved in the formation of atherosclerotic plaques in the arteries. In the innermost layer of the vessel wall (intima), LDL cholesterol is oxidized and taken up by special cells (macrophages or scavenger cells). The oxidized LDL triggers inflammation and can lead to damage to the arteries. In most patients, LDL cholesterol levels correlate very well with the ApoB concentration and provide a clear indication of the risk of arteriosclerosis.
Healthy Eating
To keep the risk of stroke as low as possible, a varied diet is recommended, which includes plenty of fruits and vegetables, whole grains, and unsaturated fatty acids. An example of this is the “Mediterranean Diet,” a diet rich in vegetables and unprocessed foods. What you should definitely avoid or reduce are saturated fats, trans fats, sugars, and salt (<6 g per day). Additionally, dairy products should be low-fat or fat-free to not elevate blood fat levels.
Regular Exercise
Physical activity helps to strengthen the cardiovascular system and reduce the risk of stroke and other cardiovascular diseases. Try to incorporate about 30 minutes of sports or exercise into your daily routine. Suitable activities include brisk walking, cycling, or swimming.
Studies show that regular physical activity can reduce the risk of stroke by 25–30%.
Non-smoking
Smoking significantly increases the risk of stroke and other serious diseases. Smoking raises blood pressure and reduces the oxygen content in the blood. Additionally, tobacco smoke contains over 4000 toxic chemicals that accumulate in the lungs or are absorbed into the bloodstream and damage the blood vessels.
A review found that smoking increases the risk of stroke three to fourfold. Even passive smoking in enclosed spaces significantly increases the risk of stroke by 1.5 to twofold.
If you smoke, you should consider quitting.
Limiting Alcohol Consumption
Too much alcohol can lead to increased blood pressure and significantly increase the risk of strokes and other diseases. A study involving 160,000 Chinese participants found that alcohol consumption contributed to 8% of all ischemic strokes and 16% of hemorrhagic strokes.
Since alcohol is a cell poison and a trigger for many other diseases, medical advice is to abstain from alcohol. The World Health Organization also recommends minimizing alcohol consumption due to the associated health risks.
Healthy Body Weight
Overweight and obesity are associated with an increased risk of high blood pressure, diabetes mellitus, and other factors that can increase the risk of stroke.
Several studies suggest that a high Body Mass Index (BMI) can increase the overall risk of stroke, particularly for ischemic stroke.
In an American study, over 21,000 doctors documented the strokes of their patients in connection with BMI over a period of 12.5 years. Participants with a BMI of ≥30 had twice the risk of ischemic stroke compared to participants with a BMI <23. For hemorrhagic stroke, the risk was even more than twice as high.
However, BMI as a sole risk factor with regard to body weight is now considered outdated. Particularly visceral fat (internal abdominal fat) is considered risky. The inner abdominal fat is particularly metabolically active and produces messenger substances that affect various processes in the body. For example, it promotes inflammatory processes and high blood pressure and favors insulin resistance. The more visceral fat there is, the greater the risk of cardiovascular diseases (e.g., arteriosclerosis, stroke, heart attack) or metabolic diseases such as diabetes.
Visceral fat can be excellently depicted and quantified by MRI imaging. Alternatively, a DEXA scan, which uses X-rays to precisely distinguish bone, muscle, and fat tissue, can determine the body fat percentage and fat distribution.
What Are Risk Factors for Stroke?
Many factors or pre-existing conditions can contribute to an increased risk of stroke.
Most of the causal factors for stroke can be influenced by us. These include:
- Lack of exercise
- Overweight
- Unbalanced diet
- High blood pressure
- Smoking
Most risk factors are based on lifestyle, genetics, and environmental factors. Ischemic and hemorrhagic strokes share many of the same risk factors, such as high blood pressure, diabetes, and high cholesterol levels. Other risk factors are specific to the type of stroke.
Important risk factors also include:
- Age: Older people have a higher risk of stroke than younger people, as they often already have atherosclerotic vascular changes. In principle, however, a stroke can occur at any age. What many do not know is that the risk of stroke is highest for infants up to the 28th day of life, even comparable to the risk in old age. About 1 in 1,000 newborns suffers a stroke.
- Cardiovascular diseases: Blood clots can be caused by coronary artery diseases, atrial fibrillation, heart valve diseases, diseases of the carotid artery, and aneurysms of the cerebral arteries. Bleeding can occur after taking blood thinners.
- Anxiety, depression, and stress can increase the risk of stroke, as they raise blood pressure and promote inflammation.
- Family history: Family predisposition and genetics also play a significant role. Your risk of having a stroke is higher if a parent or another family member has had a stroke, especially at a younger age. This is mainly because there is a predisposition for high blood pressure, diabetes, lipid metabolism disorders, or vascular diseases in the family.
- Genetics: Certain genes, such as those for lipoprotein(a), also influence the risk of stroke, as they increase the risk of arteriosclerosis, thrombosis, and inflammation. Also, the genes that determine your blood type can have an influence. For example, people with blood groups A and AB have a higher risk of suffering an ischemic stroke compared to blood group 0.
- Air quality: Various air pollutants and particles can harm the cardiovascular system. The smallest fine dust particles can penetrate the lungs and enter the bloodstream, where they can promote inflammation. Nitrogen dioxide is an irritant gas and can cause inflammation of the respiratory tract. In addition, it can impair the function of blood vessels and promote the formation of blood clots, increasing the risk of strokes. Carbon monoxide can be harmful even at lower concentrations, as it impairs the body's oxygen supply and increases the risk of heart attacks and strokes.
- Other diseases such as sleep apnea, kidney diseases, diabetes mellitus, and migraines are also contributing factors to stroke. The apneas associated with sleep apnea can lead to oxygen deficiency in the blood, which can promote inflammation, oxidative stress, and high blood pressure, all of which can increase the risk of stroke. Kidney diseases can lead to an accumulation of waste products in the blood, which can strain the cardiovascular system and increase the risk of arteriosclerosis and cardiovascular diseases, including strokes. Elevated blood sugar levels resulting from diabetes damage the blood vessels and lead to the formation of blood clots in the vessels, which in turn can lead to arteriosclerosis and promote vascular occlusion. A study found that younger people, in whom the cause of an ischemic stroke is unclear, are significantly more likely to suffer from migraines with aura (temporary visual disturbances) compared to the average population.
- Gender: Gender can also play a role in stroke risk. In younger years, men are more likely to suffer a stroke than women. This may be due to lifestyle factors (smoking, alcohol consumption, or unhealthy eating habits), and men have a greater risk of high blood pressure or diabetes. However, women generally live longer, so their stroke risk over their total lifespan is higher. Additionally, women who take birth control pills or use hormone replacement therapy have a higher risk. Women are also at a higher risk during pregnancy and in the weeks following childbirth. High blood pressure during pregnancy, for example, as part of preeclampsia, increases the risk of stroke later in life.
What Are the Precursors of a Stroke?
- Visual disturbances
- Speech and language comprehension disorders
- Paralysis (often one-sided)
- Tingling or numbness in hands, legs, arms, or one side of the face
- Dizziness
- Balance disorders
- Severe headache
A stroke typically occurs suddenly and without warning. Symptoms of a stroke include sudden confusion, speech difficulties, numbness or weakness, especially on one side of the body, facial paralysis, severe headaches, vision problems, gait disorders, dizziness, or loss of balance.
The severity of the symptoms depends on the type of stroke and the affected area of the brain.
How Long in Advance Does a Stroke Announce Itself?
The signs and symptoms of a stroke often occur very quickly and suddenly. However, they can also develop over hours or even days. This sometimes happens when a transient ischemic attack (TIA) – a temporary interruption of blood supply to the brain – appears as a precursor to the stroke.
How Do I Know If I Had a Stroke?
There are certain signs and symptoms to look out for to determine if you may have had a stroke.
A first assessment to determine if it is a stroke is provided by the so-called FAST test. FAST stands for "Face, Arms, Speech, Time". This is a quick and simple way to determine if someone has had a stroke:
- Face: Ask the person to smile and check if one side of the mouth is drooping. Very often, only one side of the face is affected in a stroke.
- Arms: Ask the person to stretch both arms forward and check if one arm sinks.
- Speech: Ask the person to repeat a simple sentence and pay attention to whether the speech is clear or incomprehensible.
- Time: If any of these anomalies occur, it is important to seek medical help immediately. Every minute counts to minimize the risk of brain damage.
Even if the symptoms appear temporary or improve, this could be a sign of a TIA, which can have serious consequences. Approximately 10% of all patients with a TIA experience a major stroke within the following 7 days.
How Can a Stroke Be Diagnosed?
A stroke is usually diagnosed through a combination of physical examination, imaging, and laboratory tests. Common diagnostic procedures include:
- Computed Tomography (CT): This is often the first imaging procedure performed when a stroke is suspected. A CT scan can help determine whether a blood clot or brain hemorrhage is present. Additionally, plaques can sometimes be seen, making CT a good option for early detection of atherosclerotic vascular changes. There is also the CT coronary calcium measurement, which can detect calcifications of the coronary arteries (coronary arteries). This determines the degree of calcification, the amount of calcium, and the effective amount of calcium. The more pronounced the calcification, the greater the likelihood that a stroke will occur within the next 5 years.
- Magnetic Resonance Imaging (MRI): An MRI provides more detailed images of the brain than a CT scan. It can be used to assess the extent of brain tissue damage and provide further information about the stroke. Also, a narrowing of the vessels (vascular angiography) such as the carotid artery and cerebral arteries can be detected using MRI.
Other tests that can be helpful in diagnosing a stroke include blood tests to check blood sugar levels, blood clotting, and other factors, as well as an electrocardiogram (EKG) to rule out arrhythmias that could lead to a stroke.
The exact diagnosis and treatment of a stroke depend on various factors. These include the type of stroke, the severity of the symptoms, and the overall health of the patient.
Conclusion
A stroke can change the lives of those affected and their families overnight and have serious consequences. However, there are several ways to reduce the risk of stroke and detect signs early.
A stroke can have various triggers. These include increased blood pressure and increased cholesterol levels, which can lead to vascular changes and thus to circulatory disorders.
Most risk factors can be influenced by a healthy lifestyle with a balanced diet, regular exercise, and the avoidance of risk factors such as smoking and excessive alcohol consumption. Regular medical check-ups and heightened awareness of the symptoms of a stroke are also crucial.
However, there are also contributing factors over which we have no control. These include gender, family history, or age. Generally, the risk is higher for infants under one year and for adults with increasing age. Hormonal contraceptives or pregnancy can also lead to an increased risk.
In the event of a suspected stroke, a quick response is important. The FAST test offers a simple way to recognize the first signs of a stroke. Furthermore, thorough diagnostics using CT or MRI and comprehensive treatment are crucial to reduce the risk of permanent brain damage and provide the best possible therapy for the patient.
Would you like to learn more about how you can prevent a stroke with MRI? Then join our waiting list, and we will inform you when it is time.






