Multiple sclerosis is a complex CNS disease with varied symptoms and progression, affecting young adults predominantly.
Multiple Sclerosis (MS) is the most common inflammatory disease of the central nervous system (CNS) in Central Europe. It is also known as the “disease of a thousand faces” because each patient experiences different symptoms with varying intensity and progression.
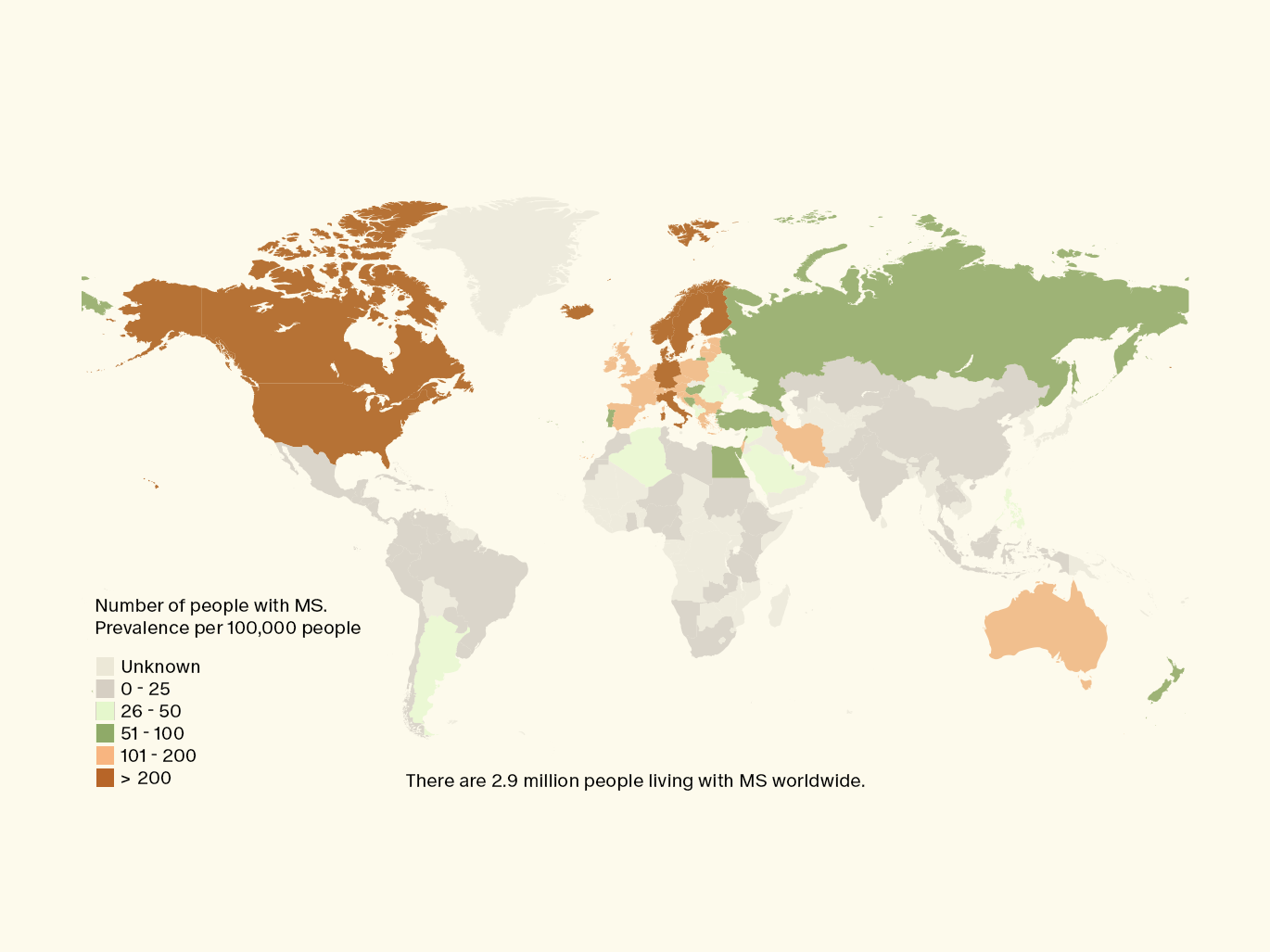
The disease typically begins in early adulthood and is usually diagnosed between the ages of 20 and 40. However, it often takes many years to reach a definitive diagnosis. Women are twice as likely to develop MS as men. Worldwide, 2.9 million people are affected by MS, with about 15,200 cases in Switzerland.
In this article, we explain the causes of MS, how it is diagnosed, and what affected individuals can do. We also explore whether it is possible to prevent the disease.
What is Multiple Sclerosis?
MS is a chronic inflammatory disease of the central nervous system in which the immune system attacks the nerve cells of the brain and spinal cord. MS can be relapsing or progressive. The first symptoms include visual disturbances, paralysis, sensory disturbances, or fatigue.
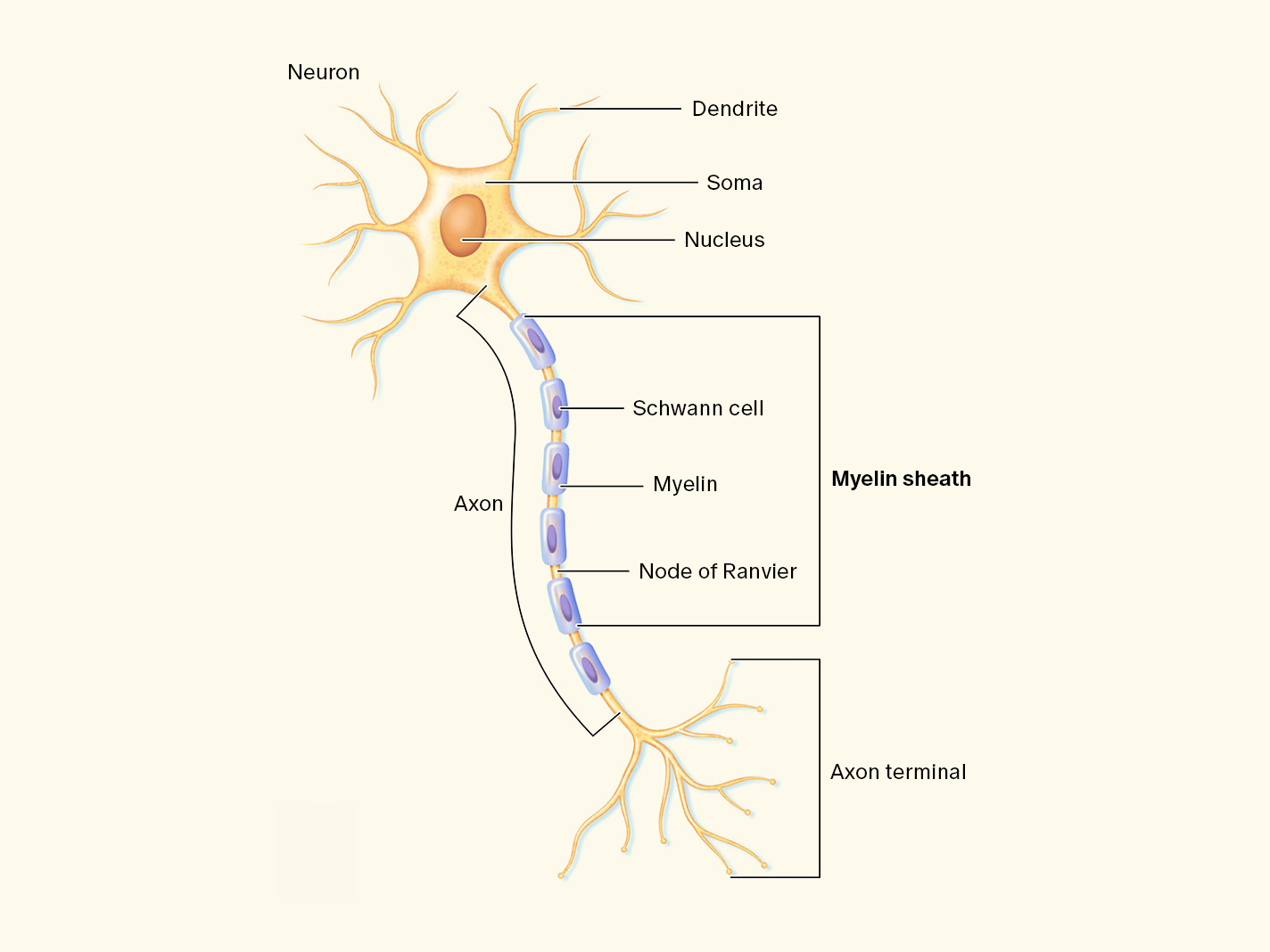
The hallmark of MS is an inflammatory reaction in the brain and spinal cord caused by the attack of the body’s own defense cells (T-cells) on the myelin sheaths of the nerves. Myelin forms the insulating layer around the nerve cells in the brain and spinal cord. The resulting demyelination initially slows nerve conduction, but gradually leads to the destruction of axons (nerve fibers), which prevents the transmission of nerve impulses and can cause significant physical and neurological impairments.
Due to the multifocal nature of the inflammation in both the brain and spinal cord, MS is also known as encephalomyelitis disseminata.
What Causes Multiple Sclerosis?
The causes of MS are not yet fully understood. However, infections with the Epstein-Barr virus, environmental factors such as smoking, vitamin D deficiency, and obesity in childhood are associated with MS. Genetic factors may also play a role, although MS is not a hereditary disease.
Viral Infections
Researchers have found that an infection with the Epstein-Barr virus (EBV) may play a role in MS pathogenesis. The virus, which causes infectious mononucleosis, is seen as a potential trigger for MS. Blood tests have detected EBV antibodies in almost all MS patients. However, not everyone with an EBV infection develops MS.
Harvard researchers discovered in a study involving US military personnel that all participants who developed MS during the study period had already tested positive for EBV in their first available blood sample.
At the end of the study, 800 of the 801 MS patients (99.9%) had been infected with EBV before the onset of MS. An EBV infection increased the risk of developing MS by about 32 times.
Vitamin D
Various studies show a link between the occurrence of MS and geographical latitude. MS is more common in populations living farther from the equator. It is argued that people with higher sun exposure (near the equator) have a lower risk of developing MS. Consequently, a connection is suspected between low vitamin D levels and an increased risk of MS as well as greater disease activity.
A Danish study linked low vitamin D concentrations in newborns with an increased risk of MS. The high prevalence of vitamin D deficiencies in pregnant women may play a role here.
Genetic Predisposition
MS is not a hereditary disease in the classical sense. However, there are genes that can contribute to the development of MS. According to the Swiss Multiple Sclerosis Society, the risk of developing MS is between 1-3% if a first-degree relative has MS.
An identical twin of an MS patient has a 25% risk of developing MS, which is 250 times higher than the general population. In Central Europe, the risk of developing MS is about 0.1%.
Smoking
Besides viral infections, smoking is also widely recognized as a significant risk factor for the development of MS. Various studies have shown that smokers have a 1.5-fold increased risk of developing MS compared to non-smokers. Smoking is also associated with a faster and more severe progression of the disease and a higher risk of transitioning from a relapsing to a chronic course.
Gut Microbiome
Research on the connection between the gut microbiome and MS is still in its early stages. However, animal experimentshave shown that genetically modified mice kept in clean but non-germ-free conditions developed MS-like episodes, whereas mice kept in germ-free conditions did not.
In another experiment, mice were given a stool sample from an MS-affected identical twin. Within 12 weeks, 60% of the animals that received the sample from the MS-affected twin developed MS-like inflammatory reactions. In contrast, only 50% of the mice that received the gut flora from the non-affected twin developed such reactions.
This suggests that certain components of the gut flora may play a role in the activation of T-cells, which in turn are involved in triggering MS.
Swiss researchers have also identified a possible autoantigen. It is a section of the enzyme GDP-L-fucose synthase, which is also produced by gut bacteria and may play a role in triggering the autoimmune reaction.
What Are the Symptoms of Multiple Sclerosis?
MS symptoms can be varied. Cramp-like paralysis (spasticity), coordination disorders, and sensory disturbances (numbness, tingling) in the arms or legs are among the first signs. Visual disturbances (due to optic nerve impairment) may also occur. Severe fatigue is also an early symptom.
Here is an overview of the most important signs:
- Visual disturbances (blurring, vision loss - often in one eye, altered color perception, double vision, etc.)
- Abnormal sensations such as tingling, burning, or numbness
- Walking difficulties: 15 years after the onset of the disease, more than 50% of MS patients have walking problems
- Leaden fatigue to the point of fatigue: up to 90% of patients suffer from fatigue
- Bladder and/or bowel dysfunction with sudden urgency, incontinence, or constipation
- Depression: MS patients are three times more likely to develop depression
Progression of MS
There is no typical course of MS. Instead, the disease is characterized by different forms of progression with various manifestations. Some patients may experience rapid worsening of symptoms, while others may live for years without relapses. Here is an overview of the different forms of progression:
Relapsing Remitting Multiple Sclerosis
Relapsing-remitting MS (RRMS) is the most common form of MS. About 90% of MS patients begin with distinct, separate relapses, interrupted by periods of remission where symptoms diminish or remain stable. Symptoms that suddenly appear during an MS relapse can completely disappear.
Secondary Progressive Multiple Sclerosis
In secondary progressive MS (SPMS), the frequency of relapses decreases, and there is a gradual clinical worsening. Regardless, additional relapses may still occur. It takes an average of 15 to 20 years for the disease to transition to this chronically progressive stage. Many MS patients, however, remain in a relapsing course and do not necessarily develop secondary progressive MS.
Primary Progressive Multiple Sclerosis
Primary progressive MS (PPMS) differs from RRMS or SPMS by the absence of relapses and remissions and is much rarer, occurring in about 10% of cases. Symptoms persist continuously and progressively worsen. While women are more often affected by the other forms, both genders are equally affected by PPMS. The diagnosis is usually made at a later age than RRMS.
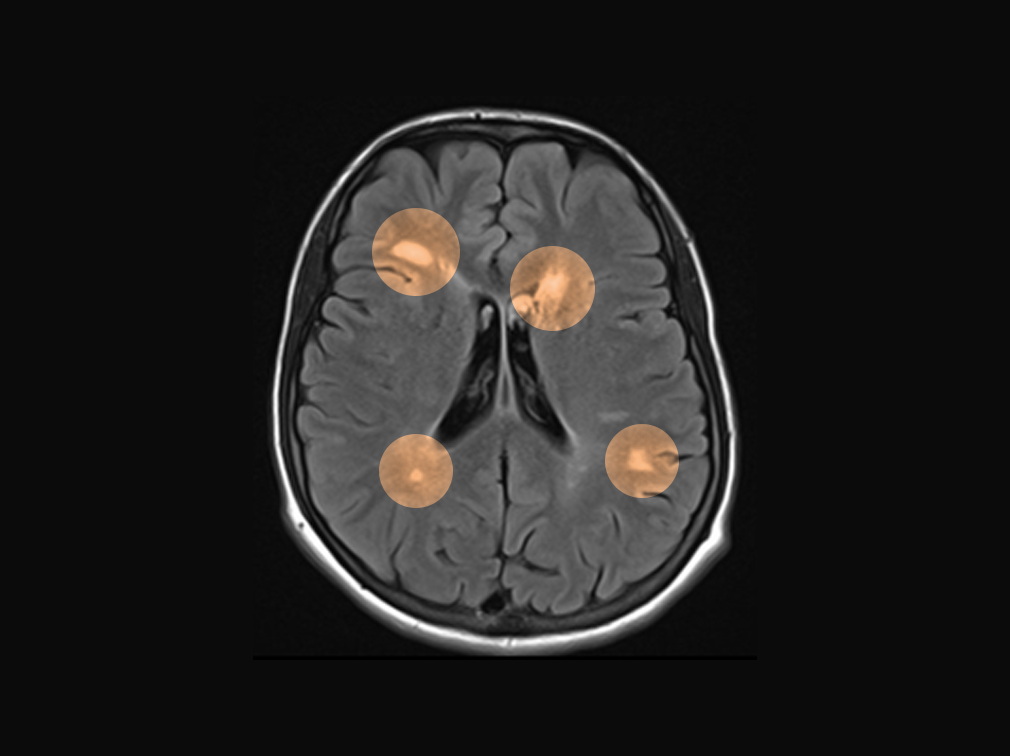
Radiologically Isolated Syndrome
Radiologically isolated syndrome (RIS) is a preclinical stage of MS, characterized by MS-typical lesions discovered incidentally on MRI without typical MS symptoms. RIS is not yet an MS disease, but it can develop into one. Upon detection of RIS, medication can reduce the MS risk by up to 72%.
How is Multiple Sclerosis Diagnosed?
The diagnosis of MS is based on the McDonald criteria, most recently updated in 2017. These criteria rely on MRI imaging, clinical examination, and laboratory values. To diagnose the disease, it must be shown that:
- The inflammatory lesions are spatially distributed, i.e., occurring in different areas of the CNS, and
- The inflammatory lesions are temporally distributed, i.e., occurring at different times.
This spatial and temporal dissemination is demonstrated through imaging techniques (MRI). Additionally, there must be recognizable clinical symptoms.
For specific symptoms that may indicate MS, further evaluation by a neurologist is performed. After a thorough medical history review, including discussing complaints and medical history, the following examinations are conducted:
- A neurological examination, assessing strength, coordination, balance, reflexes, and touch sensitivity
- MRI of the brain and spinal cord to visualize inflammatory lesions
- Lumbar puncture to collect cerebrospinal fluid (CSF) from the lumbar spine to detect specific antibodies typical for MS
- Blood tests to rule out other diseases with similar symptoms
- Possibly a nerve conductivity test, measuring visually evoked potentials to gather evidence of existing nerve damage
(old image source: https://www.leben-mit-ms.de/artikel/2023-06-21/magnetresonanztomographie_mrt_ms_untersuchung)
Preventing Multiple Sclerosis
Current knowledge suggests that preventing MS is not possible, as some risk factors such as viral infections or genetics are not modifiable. However, leading a healthy lifestyle can reduce the risk of developing MS. This includes:
- Vitamin D: A study found that spending one to two hours in the sun daily reduces the risk of MS in children by 80%. Thus, 19% of children with MS spent less than half an hour outdoors daily, compared to only 6% of children without MS.
- Sufficient Sleep: According to a Swedish study, people who slept an average of less than 7 hours per night during adolescence had a higher risk of developing MS. The same applied to poor sleep quality.
- Quitting Smoking: MS patients who smoke may transition from relapsing-remitting MS to secondary progressive MS earlier than non-smokers. A study found that those who quit smoking developed secondary progressive MS up to 8 years later than those who continued smoking.
- Exercise: A study found that people who engage in at least three hours of intense physical activity per week have a lower risk of developing MS than those who exercise less.
What Are the Treatment Options for Multiple Sclerosis?
The diagnosis of MS can create uncertainty as the course of the disease is unpredictable. Although MS is currently not curable, there are numerous medications available to alleviate symptoms and better control the course of the disease.
Currently, various medications are approved for MS therapy in Europe. For the treatment of primary progressive MS, however, only a B-cell therapy is available, which inhibits B-cells. These B-cells activate T-cells in the blood, which in turn attack the CNS.
The available treatment options can be divided into three categories:
Relapse Therapy
In the treatment of acute relapses, high-dose glucocorticoids (“cortisone”) are predominantly administered via injection over three to five days. They suppress the immune system (immunosuppressive) and improve the barrier function of the blood-brain barrier.
In severe relapses, harmful components can be removed from the blood through plasmapheresis or immunoadsorption.
Course Therapy
Course therapy, or disease-modifying therapy, aims to prevent disease progression. Unlike relapse therapy, cortisone is not suitable for long-term use due to severe side effects such as osteoporosis or diabetes mellitus.
Disease-modifying therapy is based on two principles: immunomodulation and immunosuppression, depending on the severity of the disease. Immunomodulators influence the immune response in the body, balancing immune-stimulating and immune-suppressing mechanisms. They may also help promote the rebuilding of damaged myelin sheaths and prevent scarring in the CNS.
In immunosuppression, immune cells are suppressed in their function to prevent the damaging attack on the nervous system.
Symptomatic Therapy
Symptomatic therapy accompanies the treatment of acute relapses and course therapy. It includes physiotherapy, medications to reduce spastic muscle contractions, speech therapy, psychotherapy, and the provision of aids such as walking aids or wheelchairs.
What is the Life Expectancy of Multiple Sclerosis Patients?
Multiple Sclerosis has a minor impact on life expectancy. Compared to the general population, it is shortened by 7-14 years. MS patients with a relapsing course have an average life expectancy of 77.8 years, while those with a primary progressive form have a life expectancy of 71.4 years.
Conclusion
Multiple Sclerosis is the most common inflammatory disease of the central nervous system in Central Europe. The triggers of the disease are still not fully understood. However, there are several risk factors associated with MS, including infection with the Epstein-Barr virus, smoking, vitamin D deficiency, and obesity in childhood and adolescence. Research on MS is ongoing, and the importance of the gut microbiome is gaining attention.
MS is typically diagnosed through neurological examination, MRI, and cerebrospinal fluid analysis. Blood tests and nerve conductivity measurements may also be conducted.
As varied as the symptoms can be, so too can the course of the disease. While some patients experience minimal impact on their quality of life, others may have a rapid and severe progression that affects both physical and mental health.
Although MS is currently incurable, it can be treated with various medications. Due to effective therapies, patients have only slightly reduced life expectancy compared to the general population.
CTA
If you have an increased risk due to a past EBV infection or family history, an MRI scan can provide clarity. Join our waiting list to learn more about our MRI offerings.






