Herniated disc: disc material displaces, compressing nerves. Causes include aging, poor posture, and lifestyle factors.
A herniated disc (prolapse) involves the displacement of disc material, compressing adjacent nerve roots or the spinal cord. It is a common condition that can significantly impair quality of life. Causes include degenerative changes, modifiable lifestyle factors, and genetic factors.
In this article, we will delve into the biomechanics of the spine and explain how you can prevent a herniated disc.
Key Facts
- Definition: A herniated disc involves displacement of disc material, compressing nearby nerves or the spinal cord, leading to significant discomfort.
- Importance of Discs: Discs act as "shock absorbers," providing flexibility and maintaining spacing between vertebrae.
- Causes: Degenerative changes, lifestyle factors, and genetics can contribute to a herniated disc.
- Prevention Tips: Maintain proper posture, strengthen core muscles, maintain a healthy weight, avoid prolonged sitting, quit smoking.
- Diagnosis: Typically diagnosed via MRI or CT scans, with MRI preferred for detailed images of soft tissues.
Why Are Discs So Important?
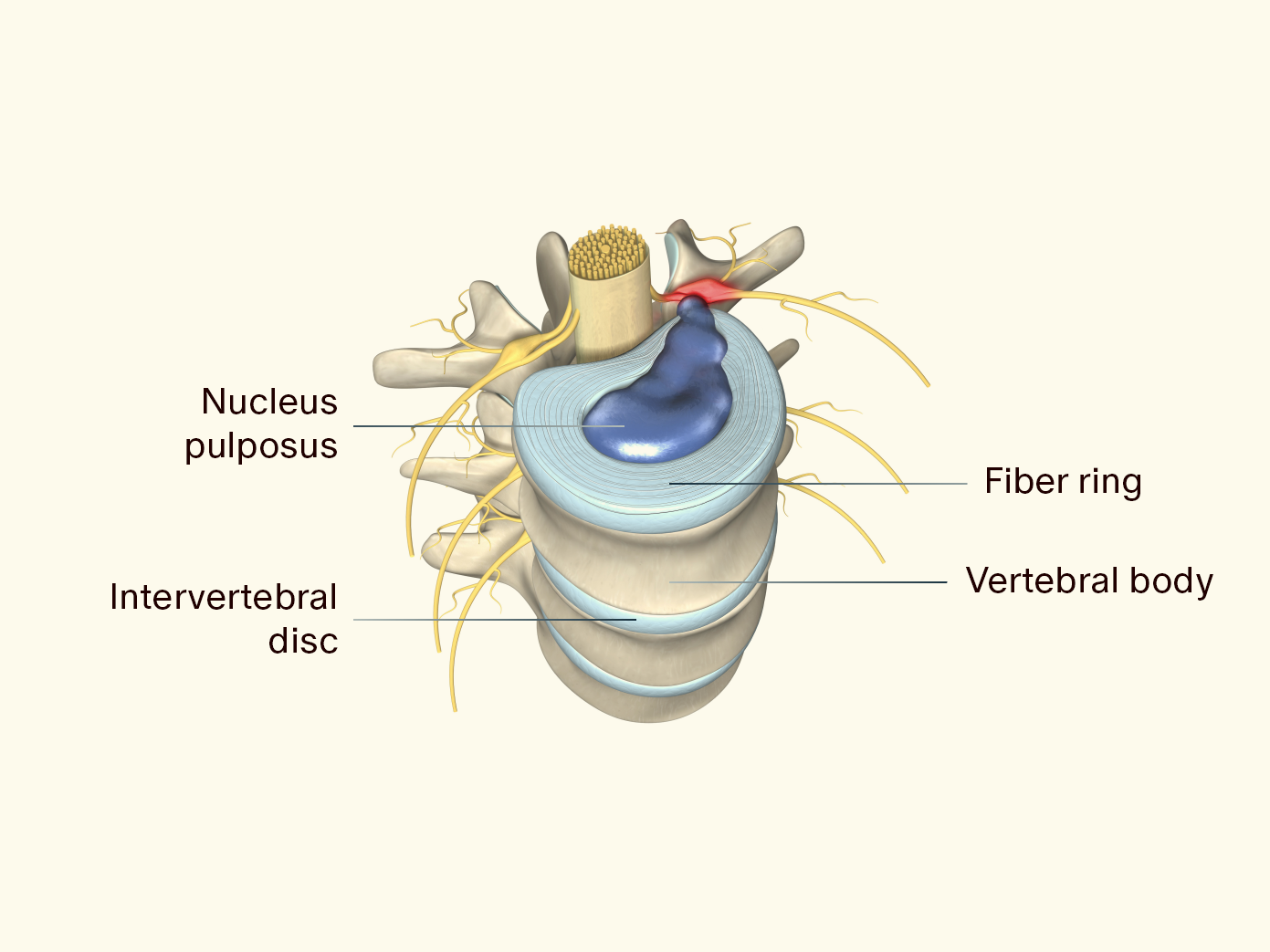
The intervertebral disc (discus intervertebralis) is located between two vertebral bodies and consists of a non-compressible soft gelatinous core (nucleus pulposus) surrounded by a fibrous ring (annulus fibrosus).
Discs function as shock absorbers, absorbing compressive forces, promoting spinal flexibility, and maintaining the distance between vertebrae. Misalignments, heavy lifting, poor posture, and lack of exercise can lead to degenerative changes in the discs and increase the risk of a herniated disc.
How Does a Herniated Disc Occur?
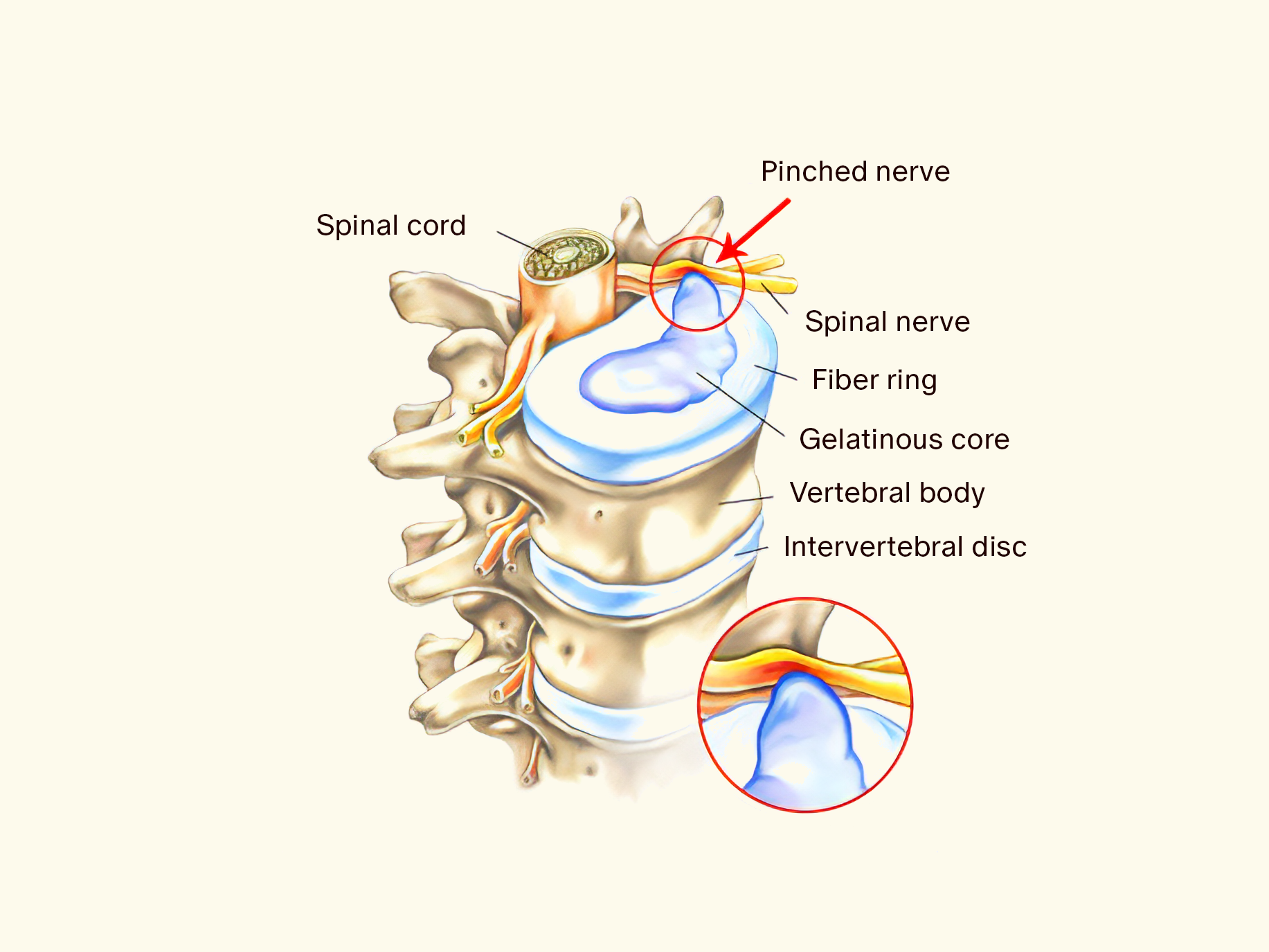
A herniated disc refers to the partial or complete tearing of the outer fibrous ring with displacement of parts of the disc into the spinal canal.
In most cases, a herniated disc is not caused by trauma, such as extreme stress from an accident or overexertion in high-performance sports. Instead, it often results from (age-related) wear and tear of the disc material. With increasing age, the water content and elasticity of the disc decrease, making it more susceptible to tears. In some cases, genetics may also be responsible. Researchers have found that increased production of the protein CILP can lead to increased instability of the discs and faster disc degeneration.
Here is how a herniated disc occurs:
- If the disc is subjected to constant high pressure, the core pushes against the fibrous ring, causing it to bulge outward and develop tears. This is called a disc protrusion and may remain unnoticed at this stage.
- If the pressure persists or increases over time, the outer fibrous ring can tear, and the gelatinous core can escape. When this happens, the body absorbs the extruded material. This is called a herniated disc.
- If disc material has already exited the spinal canal and no longer has a direct connection to the disc, it is referred to as a sequestered disc.
Herniated Disc of the Lumbar Spine
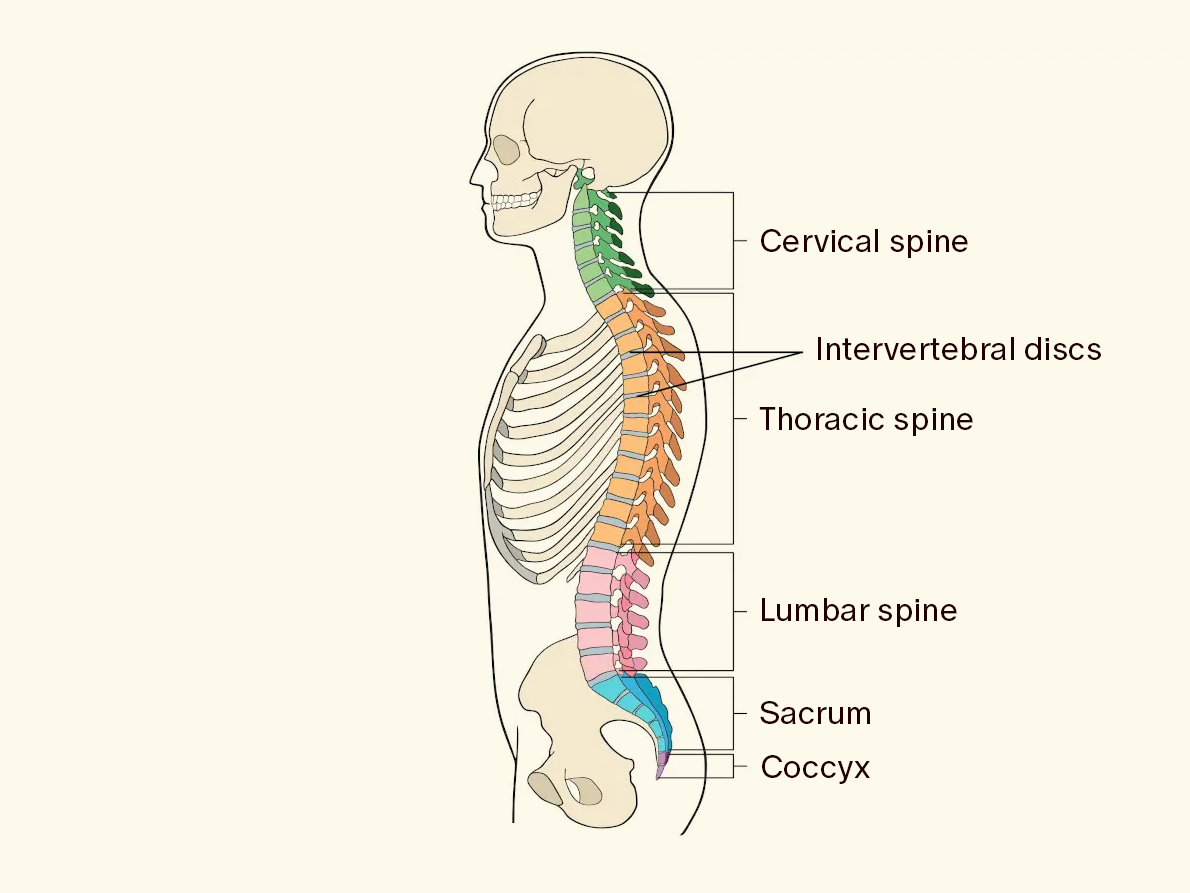
Herniated discs most commonly occur in the lumbar spine (lumbar herniated disc).
The most common cause of a lumbar disc protrusion that can develop into a herniated disc is a sedentary posture, such as in school or at a desk job.
Lack of backward movement shortens the hip flexor muscles, pulling the spine into a lordotic position. This shortens the back muscles, compressing the discs and causing a protrusion into the nerve canal. This can irritate the nerves, causing pain.
Herniated Disc of the Cervical Spine
About 10% of herniated discs affect the cervical spine, known as cervical herniated disc. A common cause of cervical herniated discs is poor posture from prolonged sitting at a desk or the so-called "smartphone neck."
Prolonged incorrect posture leads to hyperextension of the cervical spine, compressing the discs in the neck. Optimal disc function and nutrient supply require intermittent unloading. Alternating between loading (allowing waste products to exit through compression) and unloading (allowing the disc to absorb nutrients) prevents degenerative changes in the disc.
Herniated Disc of the Thoracic Spine
Thoracic herniated discs are the least common, accounting for 0.1 to 3% of all herniated discs. They most frequently affect adults between the ages of 30 and 50.
A notable aspect of thoracic herniated discs is the prevalence of calcifications or even ossifications. In a study with 167 operated patients, 58% of the extruded tissue (herniation) was found to be soft, while 42% was calcified. The reasons for these calcifications are still unclear. One cause has been described as the expansion of the nucleus pulposus, which was itself calcified.
Symptoms of a Herniated Disc
- Pain (sometimes sudden and severe)
- Tingling, especially in the extremities
- Numbness, especially in the extremities
- Weakness, especially in the extremities
- Sensory disturbances, especially in the extremities
- Neurological deficits (due to spinal cord damage)
Because a herniated disc can occur in different regions (see previous section), the symptoms also vary:
Symptoms of a Lumbar Herniated Disc
In addition to the general symptoms mentioned earlier, a lumbar herniated disc may cause back pain that radiates to the buttocks, legs, and feet. Numbness in the lower extremities is also typical. It can also irritate the sciatic nerve, leading to lower back spasms. In more severe cases, it can cause paralysis of the leg, bladder, and bowel muscles.
Symptoms of a Cervical Herniated Disc
Symptoms of a cervical herniated disc appear in the neck and shoulder area and can affect the upper arm, forearm, hand, or fingers. It manifests as numbness, tingling, and weakness in the upper extremity. It can also cause weakening or paralysis of the arm muscles.
Symptoms of a Thoracic Herniated Disc
The main symptom of a thoracic herniated disc is pain between the shoulder blades, often described as a pressure-like sensation. In some cases, the pain can spread around the chest. Coughing or sneezing can intensify the pain. Unlike a lumbar herniated disc, the pain is localized to the level of the affected vertebra and rarely radiates.
How is a Herniated Disc Diagnosed?
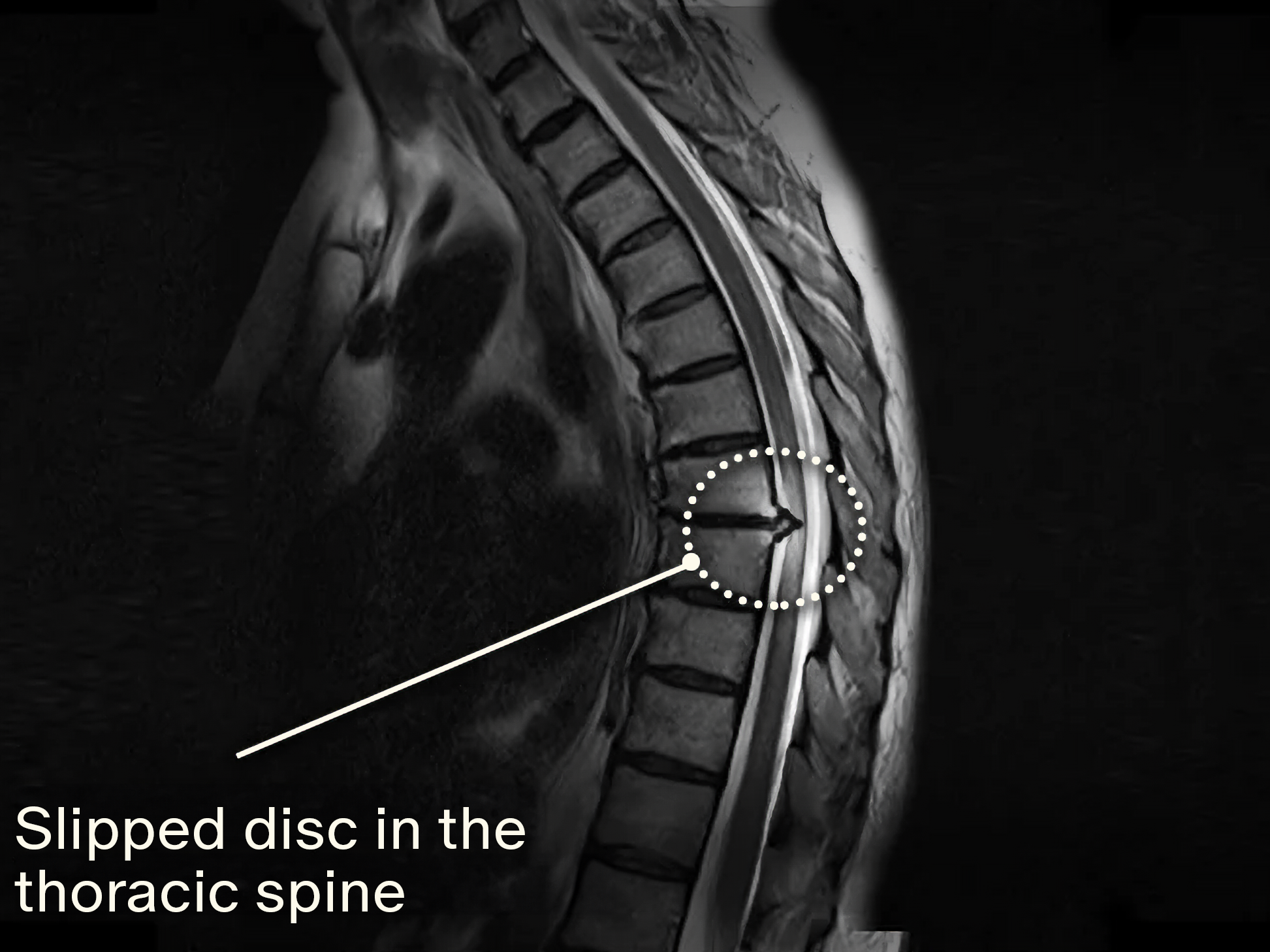
A herniated disc can be diagnosed using various methods. After a thorough medical history, the diagnosis is most commonly made using computed tomography (CT) and magnetic resonance imaging (MRI).
Diagnosis Using CT
CT is an imaging technique that provides excellent visualization of bony structures. However, the disc itself and the contact between the disc and the nerve root cannot be optimally visualized. Additionally, CT involves radiation exposure, making MRI preferable.
Diagnosis Using MRI
For herniated discs, MRI is the preferred method as it provides overlay-free sectional images of discs, spinal cord, and spinal nerves. MRI offers more detailed images of soft tissues compared to CT and can clearly show the contact between the disc and the affected nerve root, identifying the cause of symptoms.
In addition to the previously mentioned general symptoms, a herniated disc in the lumbar spine can manifest as back pain radiating into the buttocks, legs, and feet.
Numbness in the lower extremities is also typical of a herniated disc in the LWS. It may also lead to irritation of the sciatic nerve. Furthermore, muscle tension in the lower back is common. In more acute cases, paralysis of the leg, bladder, and bowel muscles may occur.
How Can I Prevent a Herniated Disc?
- Proper Posture: Ergonomic sitting and posture exercises can reduce spinal stress and lower the risk of a herniated disc. Avoiding a protective posture when experiencing back pain is essential.
- Strengthening Core Muscles: Targeted exercises to strengthen abdominal and back muscles significantly support the spine and reduce excessive disc strain. Focus on exercises that primarily train the deep muscles to stabilize the spine. A good exercise for strengthening deep muscles is the plank.
- Healthy Body Weight: A balanced diet and regular physical activity can reduce the spinal stress associated with excess weight and lower the risk of a herniated disc.
- Avoid Prolonged Sitting: Frequent breaks and ergonomic adjustments during sedentary activities reduce spinal compression and promote disc health. To avoid monotonous sitting at a desk, consider using standing desks or walking pads.
- Quit Smoking: A study confirmed that smoking increases the risk of herniated discs. Quitting smoking enhances disc nutrition and improves blood flow to spinal tissues, creating a favorable environment for disc regeneration and resilience.
What Exercises Help with a Herniated Disc?
Exercises for the Lumbar Spine
Exercise 1
- Sit on the floor and stretch your legs out.
- Slightly bend your knees and let your legs tilt to both sides.
- Grab your knees with both hands and slowly bend forward from your lumbar spine.
- Walk your hands along your legs toward your feet (if possible). This way, you can carefully pull yourself forward with your torso.
- Hold this stretch for about 2 minutes.


Exercise 2
- Sit on your heels. Lean to the right side and extend your left leg forward.
- Sit on the left side of your buttocks and try to place your left leg bent in front of you.
- Slowly approach your right heel with the right side of your buttocks to achieve a stretch in the thigh.
- If you can, lean back to tilt your pelvis further back. You can support yourself with your left forearm.
- Hold this stretch for about 2 minutes.
- Repeat the exercise on the other side by extending your right leg forward.


Exercise for the Thoracic Spine
Exercise 1
- Get into a quadruped position, with your torso and head parallel to the ground, and your abdominal muscles tensed.
- Arch your back towards the ceiling (cat stretch) and hold the position for 2 to 3 seconds, then return to the starting position.
- Repeat the exercise 15 times.


Exercise 2
- Sit on a chair and cross your arms in front of your chest.
- Roll your neck and upper back area, turning your face towards the floor for a short time, with your chin drawn to your chest.
- Keep the lower back stable.
- Repeat the exercise 30 times.

Exercise for the Cervical Spine
Exercise 1
- Sit upright on a chair.
- Move your head straight forward, keeping your gaze forward.
- Then move your head backward.
- Hold this position for 5 seconds.
- Move your head forward again.
- You can support the movement with your fingertips on your chin.
- Perform this exercise 3 times with 7 repetitions each.


Exercise 2
- Lie on your back.
- Move your head backward.
- Slightly lift the weight of your head.
- Release the position after 5 seconds.
- Repeat the exercise 7 times.

Important: Before starting targeted back exercises or training your abdominal muscles, you should first stretch your muscles and fascia to prevent further contraction.
Can Physiotherapy and Exercises Avoid Surgery?
The short answer: In most cases, yes. About 70-90% of symptomatic herniated discs are successfully treated conservatively, which includes physiotherapy or targeted back exercises. If there is no improvement after 6-8 weeks, a (minimally invasive) procedure is often recommended.
A long-term study conducted in 2021 found that a minimally invasive procedure using a catheter had the highest success rate compared to surgery or conventional therapy. In this procedure, a solution of painkillers and a NaCl-enzyme mixture is injected directly into the disc tissue irritating the nerve root. This shrinks the disc, relieving pressure on the nerve root and alleviating pain.
Conclusion
A herniated disc is a common condition that primarily affects people between the ages of 30 and 50. However, younger individuals can also suffer from disc problems. The main cause is significant stress from prolonged sitting, heavy lifting, or poor posture.
You can prevent a herniated disc by maintaining proper posture, strengthening various muscle groups, and performing stretching exercises to lengthen shortened muscles such as the hip flexor over time. Additionally, you should maintain a healthy body weight, avoid prolonged sitting, and refrain from smoking.
If you already suffer from a herniated disc, targeted exercises for different areas of the spine can help alleviate symptoms and restore functionality. Furthermore, a physiotherapist can show you targeted back exercises that are often successful and can help avoid surgery. In some cases, however, a minimally invasive procedure may be necessary, especially if there is no improvement after 6-8 weeks.
An MRI can reveal if you have a herniated disc. It can also diagnose a disc protrusion, which is a precursor to a herniated disc.








