Worried about fatty liver disease? Learn the causes, symptoms, and treatments to protect your liver and stay healthy.
Fatty liver disease (steatosis hepatis) is one of the most common liver conditions worldwide, characterised by an excessive build-up of fat within the liver cells. In Europe, around 33% of adults are affected, and in the United States, the figure rises to nearly half the population. Among people with obesity and type 2 diabetes, the prevalence is significantly higher—affecting 70–90% of this group. However, it’s not just overweight adults who develop steatotic liver disease; slim individuals and even children can be affected. Statistically, one in three overweight children has already developed a fatty liver disease.
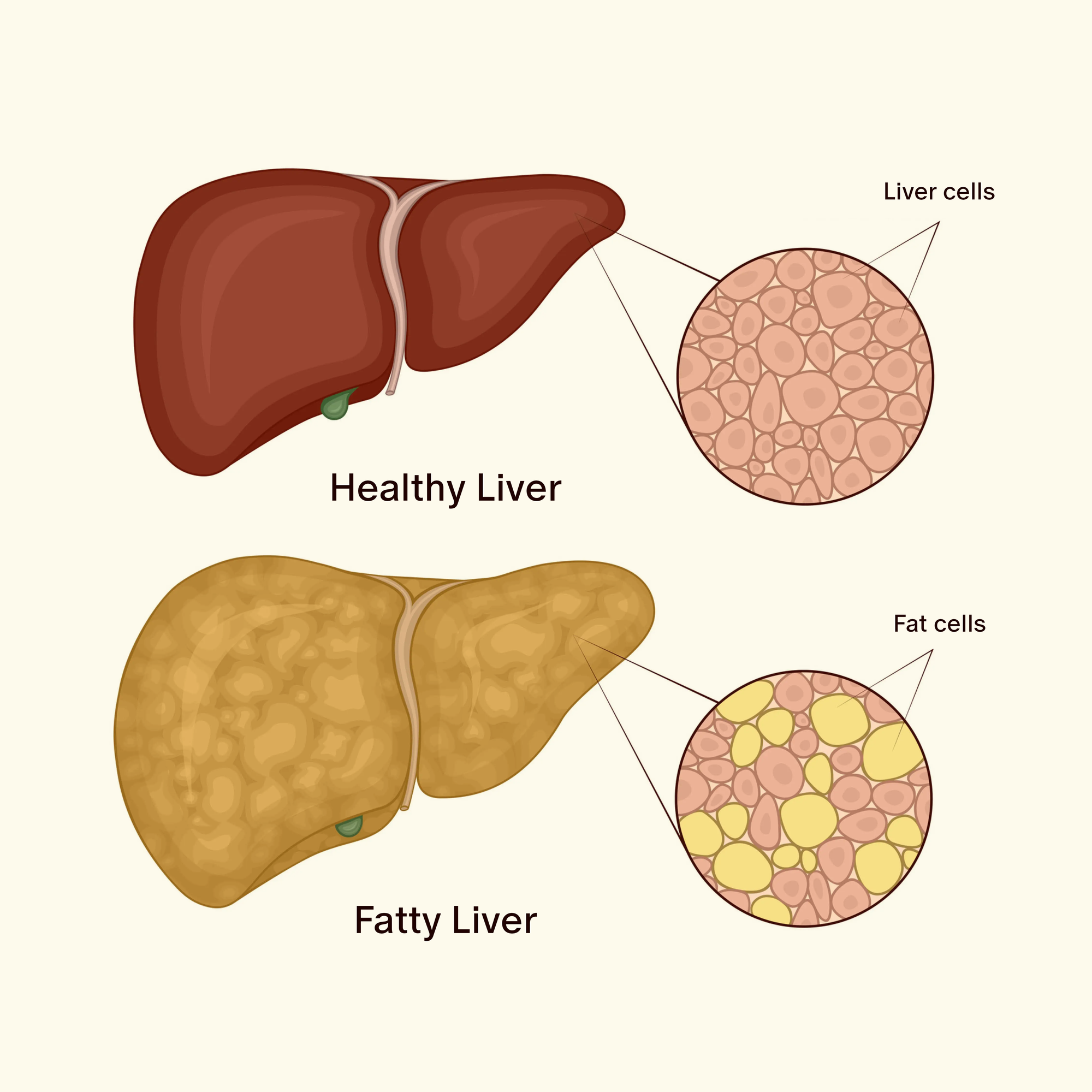
What is a fatty liver?
Fatty liver occurs when the liver is no longer able to effectively break down and eliminate fats. As a result, triglycerides in particular accumulate in the liver cells, impairing liver function. This build-up can damage the liver and prevent it from performing its essential tasks—such as removing toxins from the blood and producing bile to aid digestion. If the liver is no longer able to carry out these functions properly, there is a risk of further health complications.
For this reason, it’s crucial to detect and treat fatty liver disease at an early stage to prevent serious outcomes such as liver inflammation or liver failure.
Fatty liver disease is typically categorised into two main types of fatty liver disease: non-alcoholic fatty liver disease (NAFLD) and alcoholic fatty liver disease (AFLD). Pregnant women can also develop a specific form known as acute fatty liver of pregnancy, which can lead to postpartum haemorrhage or premature birth.
Want to stay ahead of your health?

A full-body MRI scan can detect hidden conditions like fatty liver disease early—often before symptoms appear. Schedule your preventive check-up today and take control of your well-being!
Alcoholic Fatty Liver Disease (AFLD)
Alcoholic fatty liver disease (AFLD) occurs as a result of drinking alcohol excessively over an extended period of time. The liver is the main organ responsible for breaking down alcohol. During this process, a toxic substance called acetaldehyde is produced, which can damage liver cells and lead to the buildup of excess fat in the liver.
If heavy drinking continues, a simple fatty liver disease can progress to alcoholic steatohepatitis (alcohol-related inflammation of the liver). In addition, alcohol increases oxidative stress, triggers inflammation, and activates Kupffer cells (the liver’s resident macrophages). Over time, this can lead to fibrosis (the replacement of healthy liver tissue with scar tissue) and, in more advanced cases, cirrhosis (severe scarring and destruction of the liver’s structure).
From an epidemiological perspective, AFLD is closely linked to chronic, high-level alcohol intake. Europe has the highest prevalence of this condition globally. Studies have shown that consuming 30 to 50 grams of alcohol daily over a period of more than five years significantly increases the risk of developing alcoholic liver disease (ALD). The early and potentially reversible stage of AFLD may occur in up to 90% of people who regularly consume more than 60 grams of alcohol per day.
| Amount of Alcohol (g) | Beer (5% ABV) | Wine/Sparkling Wine (12% ABV) |
|---|---|---|
| 30 g | 750 ml (1.5 large bottles) | 250 ml (2 glasses of 125 ml each) |
| 50 g | 1.25 liters (2.5 bottles) | 400 ml (3–4 glasses of 125 ml each) |
| 60 g | 1.5 liters (3 bottles) | 500 ml (4 glasses of 125 ml each) |
Non-Alcoholic Fatty Liver Disease (NAFLD)
Non-alcoholic fatty liver disease (NAFLD) is a complex liver condition that affects people who consume little to no alcohol. It is closely linked to an unhealthy lifestyle and is commonly found in individuals who are overweight or obese, as well as those with type 2 diabetes or metabolic syndrome.
Over the past few decades, NAFLD has reached pandemic proportions worldwide and is now considered the most common cause of chronic liver disease in industrialised countries. Studies show that men are more frequently affected than women, with a prevalence of around 40% in men and 26% in women.
Women with polycystic ovary syndrome (PCOS) are at significantly higher risk for developing non-alcoholic fatty liver disease (NAFLD). Elevated androgen levels, a common feature in PCOS, are associated with increased liver fat accumulation and a greater likelihood of progression to non-alcoholic steatohepatitis (NASH). Androgens can also worsen insulin resistance and contribute to abdominal fat deposition, both of which further increase the risk. Studies suggest that up to 50–70% of women with PCOS show signs of NAFLD, including those who are not overweight—a phenomenon referred to as "lean NAFLD".
One of the major concerns with NAFLD is its potential progression to non-alcoholic steatohepatitis (NASH), a more severe form of fatty liver disease characterised by liver inflammation and advancing fibrosis.
What are the signs and symptoms of fatty liver disease?
Symptoms of fatty liver disease by stage:
Early stages (often asymptomatic):
- Fatigue and general malaise
- A feeling of pressure or mild pain in the upper right abdomen
- Occasional loss of appetite
Advanced stages:
Liver inflammation (steatohepatitis):
- Pain in the upper right side of the abdomen
- Nausea and vomiting
- Jaundice (yellowing of the skin and eyes)
- Dark urine, pale stools
Fibrosis and cirrhosis:
- Swelling (e.g. in the legs or abdomen due to ascites)
- Confusion or altered consciousness (hepatic encephalopathy)
- Blood clotting problems (easy bruising)
- Rapid weight loss and muscle weakness
What causes fatty liver disease?
Fatty liver disease can have a wide range of causes and is often the result of multiple contributing factors. These include:
- Unhealthy diet:
A meta-analysis found that a high intake of red meat may increase the risk of developing fatty liver. Saturated fats found in red meat can promote inflammation and cause liver cell damage. The typical Western diet – rich in processed foods, refined grains and sugary drinks – leads to blood sugar spikes and encourages fat accumulation in the liver. The resulting weight gain further increases the risk. - Excessive alcohol consumption:
Even small amounts of alcohol can contribute to fatty liver disease. For women, just 10 grams per day (roughly 100 ml of wine), and for men, 20 grams per day (around 200 ml of wine or a pint of beer), can lead to fat build-up in the liver. However, there is no “safe” or health-neutral amount of alcohol – every drop is potentially harmful, which is why alcohol consumption is generally discouraged. - Obesity:
Studies have shown a strong link between body mass index (BMI) and the risk of fatty liver disease. Compared to individuals with a normal BMI, those with a higher BMI were 4.1 to 14 times more likely to develop the condition. People with a BMI up to 22 have a lower risk. The risk doubles from a BMI of 24.5, and is six times higher at a BMI of 28.6 or above. - Body fat percentage and abdominal fat:
Although BMI is a helpful indicator of weight status, it doesn’t account for body composition. More important are total body fat percentage and, in particular, abdominal (visceral) fat. Visceral fat can promote inflammation and insulin resistance, both of which contribute directly to the development of fatty liver. Body fat percentage shows the proportion of fat relative to total body weight. A high body fat percentage – even in people with a normal BMI – can still pose a significant risk. - Lack of physical activity:
People who sit for more than eight hours a day are at increased risk of developing fatty liver disease. This means physical inactivity can be a risk factor in its own right, regardless of weight or diet. - Medications:
Certain medications can trigger or worsen fatty liver disease. For example, steroid hormones may intensify the processes that lead to steatohepatitis (inflammatory fatty liver disease), accelerating disease progression. Other drugs – such as tamoxifen (used to treat breast cancer) or irinotecan (a chemotherapy agent) – may exacerbate or uncover an existing but previously undiagnosed fatty liver condition. - Hepatitis C:
Fatty liver is more common in people with chronic hepatitis C than in the general population. Prevalence in this group ranges from 40% to 86%. - Genetic factors:
There is strong evidence that fatty liver can run in families. However, this does not necessarily mean that the disease will develop. Recent studies have confirmed that hereditary forms of fatty liver disease do exist – for instance, involving mutations in the ABHD5 gene. Since the development of fatty liver is multifactorial, both genetic predisposition and environmental influences are likely to play key roles.
What does a fatty liver look like?
A fatty liver is often enlarged and appears paler or yellowish due to fat accumulation. Its surface may be uneven or nodular. As the disease progresses, the liver can become pathologically altered – hardening and scarring – which may eventually impair liver function to the point where a liver transplant becomes necessary.
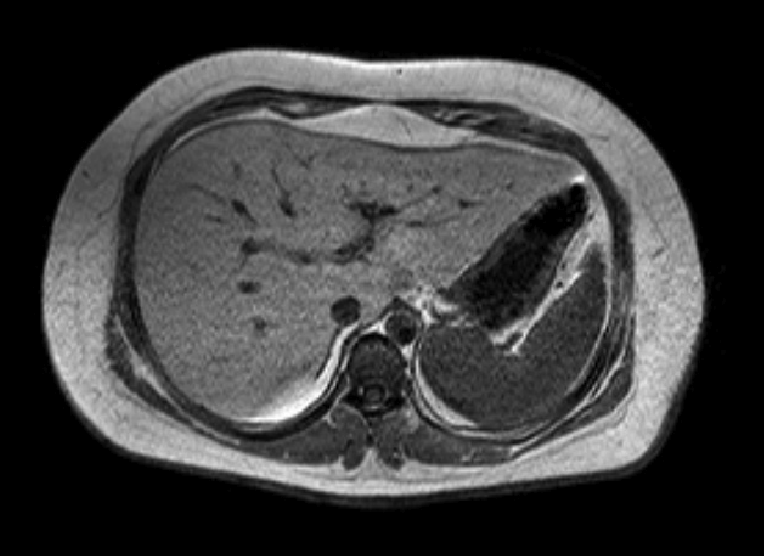
Fatty Liver on MRI
Fatty Liver on CT Scan

How is fatty liver disease diagnosed?
Medical History (Anamnesis)
Your healthcare provider will ask about current symptoms, your medical history, and potential risk factors such as type 2 diabetes or hepatitis C. A family history of nonalcoholic fatty liver disease may also suggest a genetic component.
Physical Examination and Blood Tests
This includes calculating the Body Mass Index (BMI), measuring waist circumference, and checking blood pressure.
Blood tests are a central part of diagnosing fatty liver disease and include:
- Liver function tests, especially liver enzymes such as GGT, AST (GOT), and ALT (GPT), to assess how well the liver is working
- Full blood count, to evaluate general health and detect inflammation or anemia
- Lipid profile (triglycerides, total cholesterol, HDL, LDL), to assess fat metabolism
- Fasting blood glucose and HbA1c, to check for insulin resistance or type 2 diabetes
- Hepatitis B and C screening, to rule out viral causes of liver disease
- Ferritin and transferrin saturation, to assess iron metabolism
- Liver synthesis parameters (e.g., albumin, INR), which are also part of a comprehensive liver function test panel
A particularly helpful tool is the Fatty Liver Index (FLI), which combines BMI, waist circumference, GGT, and triglyceride levels to estimate the likelihood of fatty liver disease.
Imaging Tests
Ultrasound was once the standard method for imaging fatty liver. In this scan, fatty liver tissue appears brighter due to its higher density, and liver enlargement can also be detected.
However, ultrasound is now considered inaccurate and has largely been replaced by elastography. Elastography is a painless method that measures tissue stiffness to detect conditions such as tumours or fibrosis. The scan – performed using ultrasound or MRI – takes just 2–3 minutes and can assess both liver fat content and any hardening of the tissue. It allows for accurate determination of disease stage and liver changes.
Magnetic Resonance Imaging (MRI) is also suitable for differentiating between the various stages of fatty liver in greater detail.
Liver Biopsy
A liver biopsy remains the gold standard, especially for distinguishing between simple steatosis and steatohepatitis. However, due to its invasive nature, it is not always indicated.
How is fatty liver treated?
There is currently no specific medication approved for the treatment of fatty liver disease. Promising approaches in clinical research include GLP-1 receptor agonists (which promote weight loss and improve insulin sensitivity) and FGF19 analogues (which affect bile acid metabolism). These treatments are still under clinical investigation.
At present, the most effective way to counter fatty liver and improve liver health is through prevention. This primarily involves lifestyle changes, including a healthy diet, regular physical activity, and abstinence from alcohol.
It is also essential to treat any underlying conditions that may contribute to fatty liver – such as diabetes, insulin resistance, or obesity – appropriately and consistently.
How can fatty liver be prevented?
Fatty liver can generally be prevented through the right nutrition and sufficient physical activity. The following measures can help:
- High-protein diet: Studies suggest that certain proteins may help reduce fat deposits in the liver. For instance, overweight women who consumed 60 grams of whey protein daily saw a 20% reduction in liver fat within just four weeks.
- Foods with a low glycaemic index: These cause a slower rise in blood sugar, preventing sharp insulin spikes that could promote fat storage in the liver. Suitable options include legumes, whole grains, nuts, and seeds.
- Healthy fats: Omega-3 fatty acids support the body’s ability to use insulin more effectively, allowing cells to absorb sugar more efficiently and reducing fat production and storage in the liver. These healthy fats include fatty fish, nuts (especially walnuts), flaxseeds, extra virgin olive oil, and avocados.
- Fewer meals per day: To help prevent fatty liver, it's recommended to eat no more than three meals per day, with at least five hours between meals. Snacks or small in-between meals should be avoided, as each one triggers insulin release. Researchers from the University of Tübingen (Germany) also found that intermittent fasting may help prevent liver inflammation and liver cancer.
- Fruits and vegetables: All types of fruit and vegetables can support liver health. Particularly beneficial are low-starch vegetables and low-sugar fruits, such as lettuce, cucumber, tomato, aubergine (eggplant), berries, and citrus fruits.
- Bitter compounds: Bitters stimulate bile flow and support the liver’s detoxification processes. They also reduce food cravings. Good sources include artichokes, radicchio, and chicory, and they can also be taken as a spray.
- Fibre: Dietary fibre supports gut health, which positively affects blood values and strengthens liver function. Great sources include legumes (which also offer plant-based protein), carrots, parsnips, and leafy green vegetables.
- Exercise: Studies show that 150 minutes of moderate exercise per week can significantly reduce liver fat in patients with fatty liver disease, while also improving liver health, physical fitness, and general well-being. Combined endurance and strength training is particularly effective in reducing liver fat. Even after just four weeks, it can lead to a significant reduction in intrahepatic fat. A systematic review of 21 randomised controlled trials involving 1,530 patients confirmed that this type of exercise has a rapid and positive impact on liver health.
What is the typical course of fatty liver disease?
The progression of fatty liver disease can vary greatly. In many cases, it remains asymptomatic for a long time. However, the disease may develop from a mild health problem into life-threatening complications, including liver inflammation, liver cancer, or liver failure:
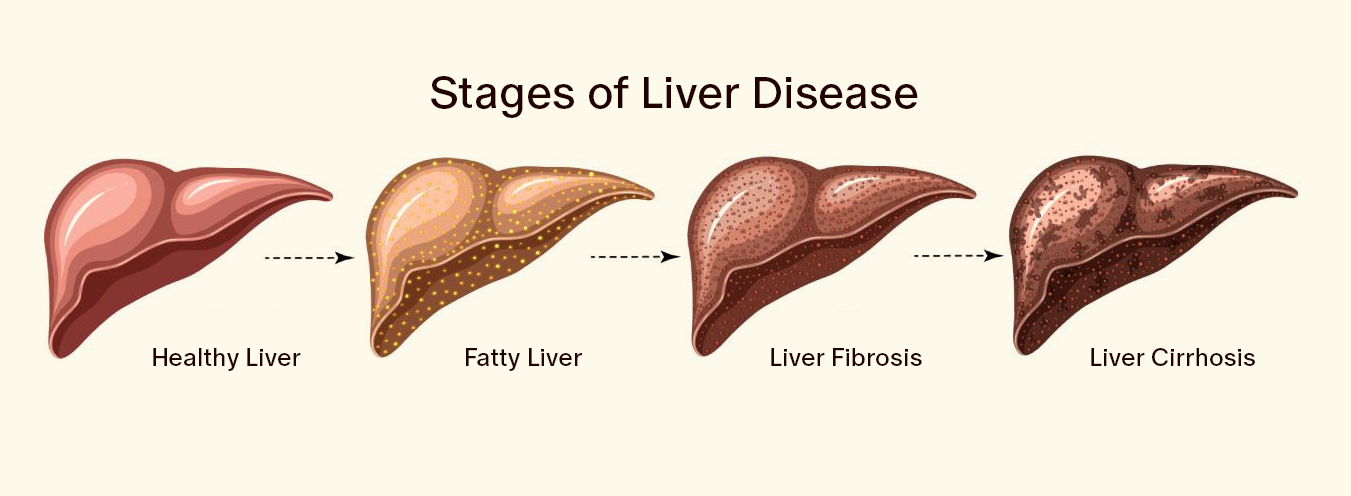
- Liver inflammation (Hepatitis):
Non-alcoholic steatohepatitis (NASH) can develop from simple fatty liver (steatosis) when fat deposits cause inflammation and damage to liver cells. This inflammation can progressively impair liver function. - Liver scarring (Fibrosis):
Chronic inflammation and damage from fat accumulation may lead to fibrosis, the formation of scar tissue in the liver. Over time, this scar tissue replaces healthy liver cells, disrupts the liver’s normal structure, and may cause lasting liver damage. - Liver cirrhosis:
In this advanced stage, the liver is severely scarred. This impairs blood flow and liver function significantly. Unlike hepatitis or early fibrosis, cirrhosis is irreversible. It can result in liver failure, portal hypertension (increased pressure in the portal vein), and complications such as ascites (fluid accumulation in the abdomen) and hepatic encephalopathy (confusion and altered consciousness). - Liver cancer:
Hepatocellular carcinoma (HCC) is a possible outcome of advanced fatty liver disease, especially in patients with cirrhosis. HCC is one of the most common cancers in people with cirrhosis, and the prognosis is often poor if the cancer is not detected early. - Liver failure:
Liver failure represents the final stage of liver disease, where the liver can no longer perform its essential functions—such as detoxification, clotting factor production, and metabolic regulation. Liver failure is life-threatening and often requires a liver transplant.
Risks and complications of fatty liver disease
If left untreated, fatty liver disease can lead to a number of serious secondary conditions and complications. These do not affect only the liver itself, but also impact the entire metabolic system and other organs. The main complications include:
- Cardiovascular diseases:
Individuals with fatty liver disease are at increased risk of cardiovascular conditions such as coronary heart disease, heart attack, and stroke. Fatty liver is frequently associated with metabolic syndrome, high blood pressure, and type 2 diabetes, all of which further heighten cardiovascular risk. - Type 2 diabetes:
There is a strong link between fatty liver and insulin resistance, which significantly increases the risk of developing type 2 diabetes. Diabetes, in turn, can lead to additional complications such as kidney failure, cardiovascular disease, and nerve damage. - Metabolic syndrome:
Fatty liver disease is often a component of metabolic syndrome, a cluster of conditions including insulin resistance, hypertension, dyslipidaemia (elevated blood lipid levels), and abdominal obesity. Metabolic syndrome increases the risk of heart disease, stroke, and type 2 diabetes. - Kidney dysfunction:
Chronic liver diseases such as fatty liver can raise the risk of renal impairment, potentially leading to chronic kidney disease. - Sleep apnoea:
Fatty liver disease, particularly in individuals with obesity, is associated with obstructive sleep apnoea, a condition characterised by intermittent pauses in breathing during sleep. - Gallbladder disease:
Fatty liver can increase the risk of gallstones, as disturbances in fat metabolism can affect the production and composition of bile. Gallstones may lead to biliary colic and cholecystitis (inflammation of the gallbladder).
Frequently Asked Questions
Can a fatty liver go away on its own?
Yes, in its early stages, fatty liver disease can regress if the underlying causes are addressed — particularly through achieving a healthy weight and increased physical activity. In cases of overweight or obesity, a weight loss of 7–10% is recommended to support the gradual regeneration of the liver.
Can dietary supplements help treat fatty liver disease?
Certain supplements may help support liver health in people with fatty liver disease, especially when combined with lifestyle changes. Vitamin E, omega-3 fatty acids, and vitamin D have shown potential in reducing liver fat and inflammation, particularly in non-alcoholic fatty liver disease (NAFLD). Other supplements like silymarin (milk thistle), berberine, and N-acetylcysteine (NAC) may improve insulin sensitivity, oxidative stress, and liver enzyme levels. However, supplements are not a cure and should always be used under medical guidance, as part of a broader treatment plan that includes diet, exercise, and reduced alcohol use.
Is a fatty liver dangerous?
A simple fatty liver (steatosis) is usually not dangerous. However, if left untreated, it can progress to steatohepatitis (fatty liver inflammation), which may lead to liver fibrosis (scarring) and ultimately cirrhosis. Cirrhosis is a serious condition that significantly impairs liver function and increases the risk of liver failure and liver cancer.
Conclusion
Fatty liver disease involves the accumulation of fat within liver cells, leading to a gradual fatty degeneration of the liver tissue. As the condition progresses, inflammation and scarring (fibrosis) may occur, which can severely impair liver function.
Fatty liver disease is a complex, multifactorial condition with a high global prevalence. While alcoholic fatty liver disease is strongly associated with excessive alcohol use, non-alcoholic fatty liver disease (NAFLD) is more common in patients with overweight, type 2 diabetes, and metabolic syndrome. Both forms, if not treated in time, can lead to severe complications such as cirrhosis and liver cancer.
Prevention and treatment are primarily based on lifestyle modification, especially for non-alcoholic fatty liver disease. In contrast, abstinence from alcohol is the cornerstone of treatment for alcoholic fatty liver.
You want to take better care of your health and identify potential health risks early? Then book your free consultation with us today.









