Colorectal cancer: third most common cancer. Early detection and screening improve survival. Learn prevention methods.
According to data from the Swiss Cancer League, colorectal cancer accounts for 10% of all cancer cases, making it the third most common cancer among men and women.
It's important to know that the common term "colorectal cancer" usually refers specifically to colon cancer, meaning colon carcinoma and rectal carcinoma (medically referred to as colorectal carcinoma). This is because small intestine cancer is much rarer, accounting for less than 1% of all new cancer cases. In this article, we will focus on colon cancer.
Colorectal cancer generally develops after the age of 50, with more than half of cases being diagnosed after the age of 70. It's important to emphasize that many diseases are present long before a diagnosis is made. Although colorectal cancer is the third most common cancer, it accounts for only 10% of all annual cancer-related deaths, meaning it is not statistically one of the most aggressive tumors. The five-year survival rate across both genders after diagnosis is 69%.
A significant reason for this is that the early detection of colorectal cancer through regular screening has vastly improved. Especially when cancer is detected in Stage 1, the chances of successful treatment are very high: The five-year survival rate is over 90%.
As with all cancers, regular screening is crucial: The earlier the cancer is detected, the better and simpler the treatment will be. To help you decide how best to take preventive measures for yourself, we will provide an overview of all the important colorectal cancer screening methods.
What Screening Methods Are Available for Colorectal Cancer?
There are three standard screening methods for colorectal cancer:
- Fecal Occult Blood Test (FOBT)
- Colonoscopy
We will explore these options in more detail below.
At What Age Is Colorectal Cancer Screening Recommended?
If no factors for increased risk are present, both women and men are recommended to begin regular check-ups for colorectal cancer screening starting at age 50.
A regular check-up means either having a fecal occult blood test (FIT) every two years or a colonoscopy every ten years. For women, a colonoscopy is recommended starting at age 55, as they tend to develop colorectal cancer later than men.
Below, we will introduce the two main screening methods for colorectal cancer.
Fecal Occult Blood Test (FOBT)
This test is quick, non-invasive, and painless. A stool sample is analyzed in a laboratory for the presence of blood, which is usually not visible to the naked eye. The presence of blood may indicate cancerous growths (tumors) in the colon.
If blood is detected, it does not always indicate cancer. The blood could also be due to chronic inflammatory bowel diseases, hemorrhoids, or benign polyps in the colon. However, benign polyps are often precursors to cancer.
Therefore, a fecal occult blood test does not diagnose cancer but serves as an initial indication of potentially concerning results.
Colonoscopy
A colonoscopy involves a physician (usually a gastroenterologist) inserting a flexible tube (endoscope) with a camera into the colon. This allows for the examination of the entire colon.
There is also the option of a sigmoidoscopy, a "small colonoscopy" in which only the last 40-60 centimeters of the colon are examined. Sigmoidoscopy is shorter and less uncomfortable than a full colonoscopy, but it only detects about two-thirds of all colorectal tumors.
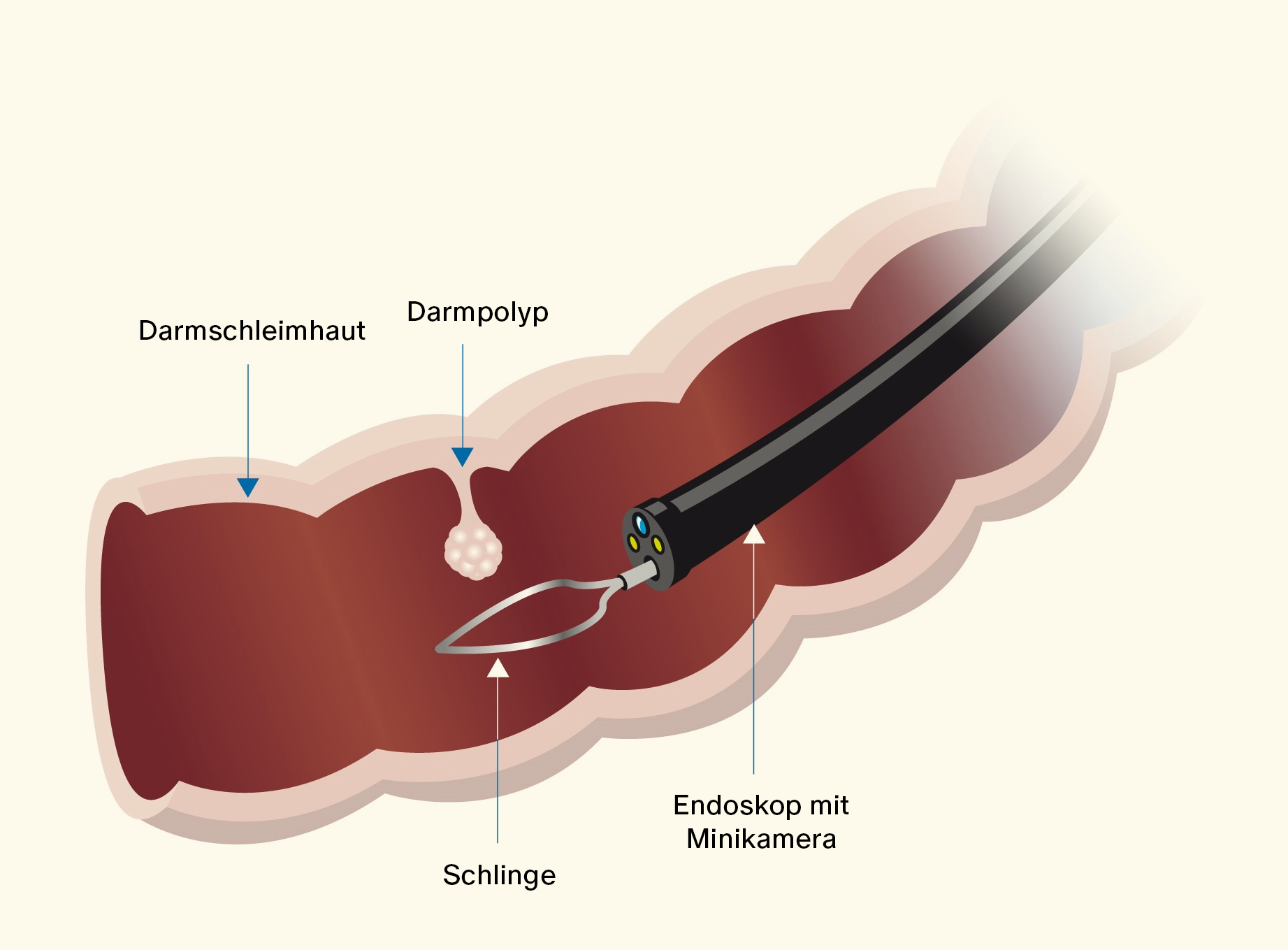
In both types of colonoscopy, the camera inserted into the colon transmits images to a screen, allowing your doctor to detect colorectal cancer with high accuracy. Colon polyps—benign growths of the mucous membrane—can be removed during the procedure. This is advisable because even benign polyps can turn into malignant tumors.
A colonoscopy is usually performed under sedation, meaning you are given medication and sleep during the procedure. Additionally, your colon must be completely empty to ensure that nothing obscures the images. Therefore, it is important to drink plenty of fluids the day before and on the day of the colonoscopy. The day before, you must take a laxative.
What Are the Benefits of Regular Colorectal Cancer Screenings?
Regular screenings for colorectal cancer offer several benefits:
- Improved Treatment Options: Early detection of a tumor significantly increases the chances of successful cancer treatment.
- Halved Mortality Rate: Since colorectal cancer can be detected and treated at an early stage, the risk of death for individuals under 80 is reduced by half, according to Swiss Cancer Screening.
- Prevention of Colorectal Cancer: During a colonoscopy, polyps (growths) can be removed before they develop into cancer.
- Improved Quality of Life: Advanced colorectal cancer can have severe consequences, which early detection usually prevents. With early diagnosis, additional treatments like chemotherapy may be avoided.
Overall, regular screenings greatly reduce the risk of colorectal cancer and its potential impact.
How Can I Reduce the Risk of Developing Colorectal Cancer?
You can effectively reduce your risk of colorectal cancer by making certain lifestyle choices.
While advanced age and hereditary factors (about 10-15% of colorectal cancers are hereditary) play a role, a healthy lifestyle can help protect against the development of colorectal cancer and even slow the growth of cancer cells.
A healthy lifestyle includes:
- Regular physical activity
- Avoiding alcohol consumption
- Not smoking
- Limiting processed food intake
- Maintaining a healthy weight
Additional Prevention Tips
There are various approaches to preventing colorectal cancer. Here are some important points:
- Screening and Early Detection: Regular screening, particularly starting at age 45 or earlier for those with a family history of colorectal cancer, is key. Colonoscopies are the most effective method for detecting polyps that can develop into cancer.
- Diet: A diet rich in fiber helps reduce the risk of colorectal cancer. Incorporating plenty of fruits, vegetables, and whole grains is recommended. Anti-inflammatory diets, such as the Mediterranean diet, which is rich in vegetables and low in processed foods, are especially beneficial.
- Anti-inflammatory Measures: Chronic inflammation can increase the risk of cancer. Taking anti-inflammatory medications, such as aspirin, in consultation with a doctor, can be a preventive approach.
- Microbiome Health: A healthy and diverse microbiome may reduce cancer risk. A diet rich in prebiotics and probiotics (e.g., fermented foods) can support good gut bacteria.
- Genetic Testing: For those with a family history of colorectal cancer or known genetic mutations, genetic testing and counseling can help assess individual risk and recommend appropriate preventive measures.
Aside from lifestyle changes, regular screening remains the most effective way to prevent colorectal cancer.
In most Swiss cantons, colorectal cancer screening is covered by insurance starting at age 50 (age 55 for women), with earlier screenings available for those with a family history. The costs for a fecal occult blood test (every two years) and colonoscopy (every ten years) are covered by the Swiss Mandatory Health Insurance (OKP), including the co-pay, while the annual deductible does not apply.
By combining these strategies, you can significantly reduce your risk of colorectal cancer while promoting overall health.
Conclusion
As the third most common cancer, colorectal cancer has a high survival rate primarily because it can be treated and even cured when detected early.
This makes regular screenings essential.
A colonoscopy can actively prevent tumor development by removing polyps. Additionally, a healthy lifestyle significantly reduces the risk of developing colorectal cancer in the first place.
Most importantly, you should take advantage of early detection screenings and sign up for your canton’s colorectal cancer screening program.
If you're interested in a full-body check-up, feel free to schedule a free consultation with us.








