Learn about cancer statistics in Switzerland: increasing cases but declining mortality, leading to better survival outcomes.
Cancer in Switzerland: An Overview
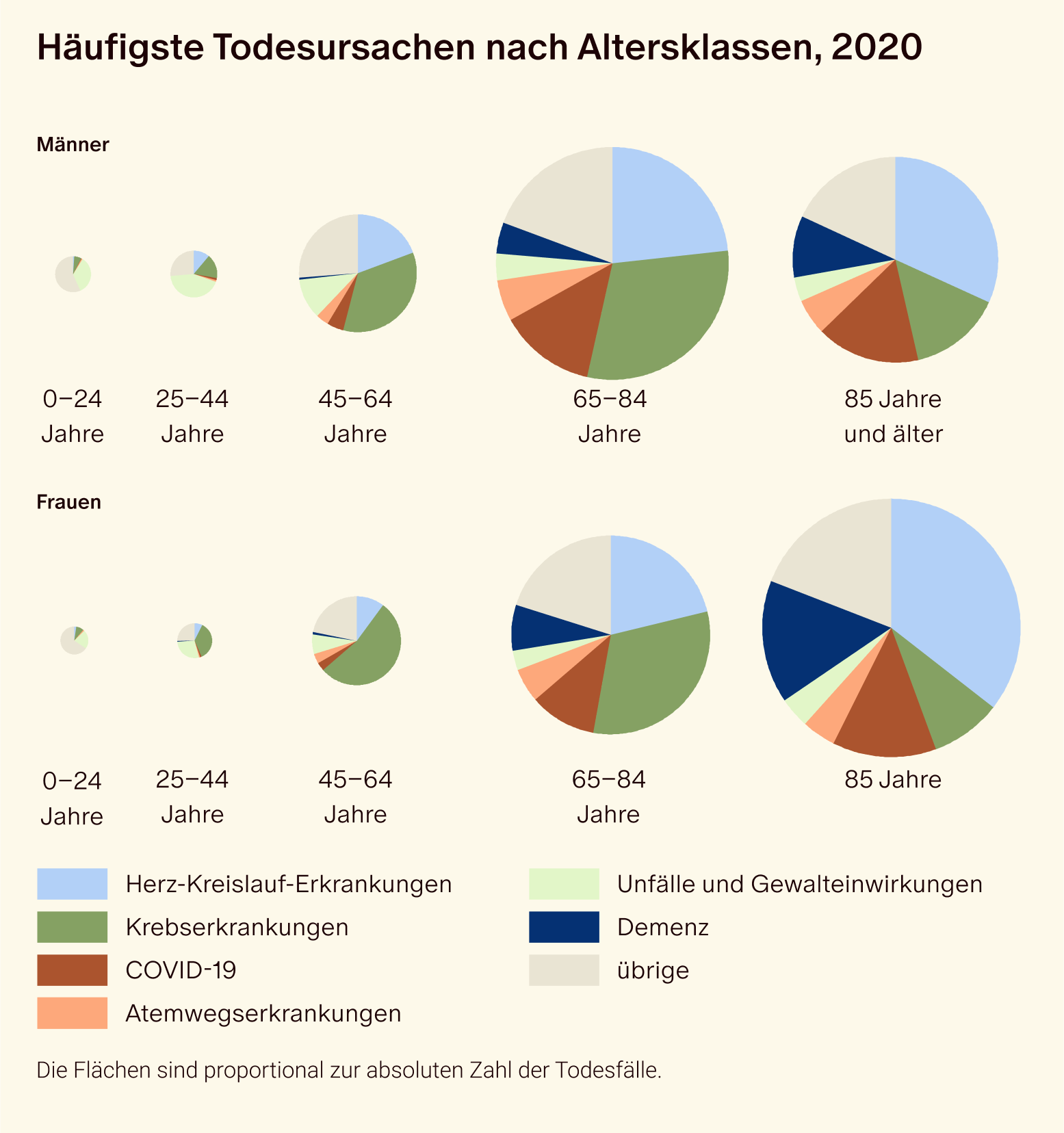
Statistically, one in five people in Switzerland is diagnosed with cancer before the age of 70. With approximately 43,000 new cases and 17,000 deaths per year, cancer is the second leading cause of death in the country, after cardiovascular diseases. Among men aged 45 to 84 and women aged 25 to 84, cancer is even the leading cause of death.
However, there has been progress: Compared to 2017, cancer mortality has decreased, and cancer patients now have a higher life expectancy on average.
The following data is largely sourced from the Cancer Report 2021, which is published every five years by the Federal Statistical Office (BFS), the National Cancer Registry (NKRS), and the Childhood Cancer Registry (KiKR).
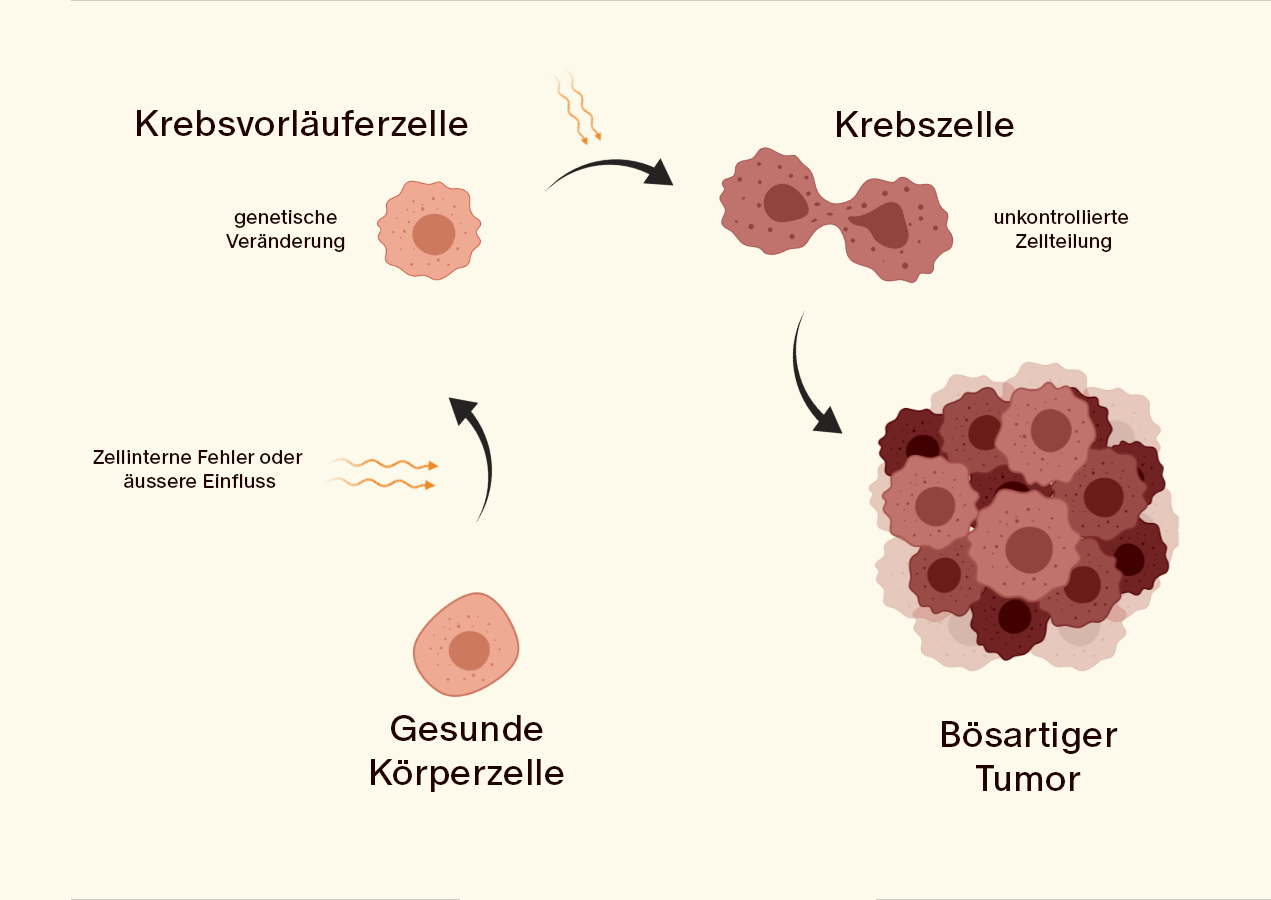
How does cancer develop? -> Info Box
Cancer develops when the genetic material (DNA) of a single cell changes. This change can be caused by various factors, such as genetic predisposition or external influences (e.g., pollutants, radiation). This alteration of the DNA leads to disruptions in normal cell functions, which results in uncontrolled cell growth and the formation of a tumor. The tumor can grow locally, invade surrounding tissues (infiltration), and form metastases, i.e., secondary tumors in other organs of the body.
Increase in New Cancer Cases in Switzerland
Between 2013 and 2017, an average of 23,100 new cancer cases in men and 19,650 new cancer cases in women were diagnosed annually in Switzerland. This represents an 8.5% increase compared to the period from 2008-2012. For the year 2021, researchers estimated 48,300 new cases, which could lead to another increase by 2024.
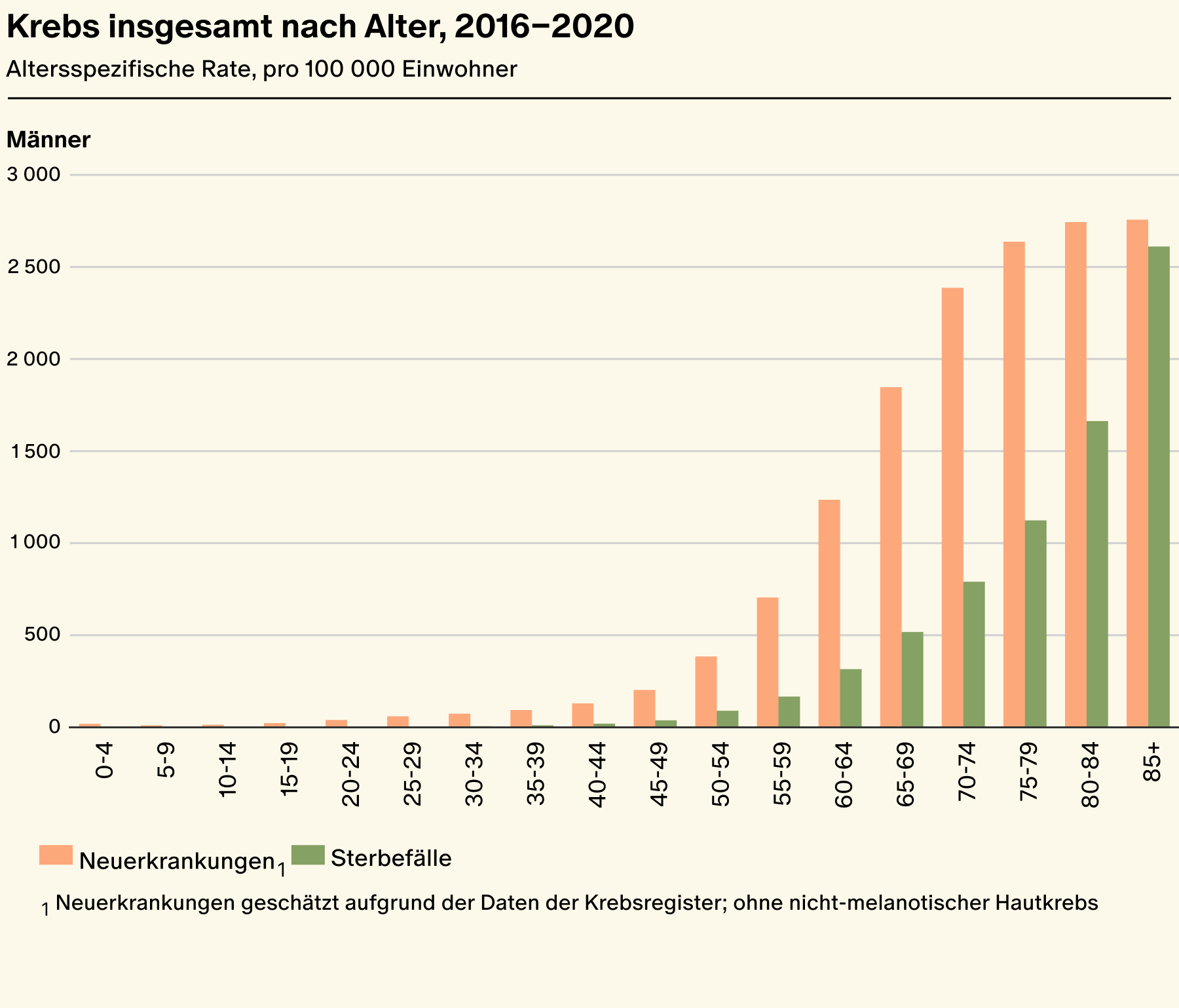
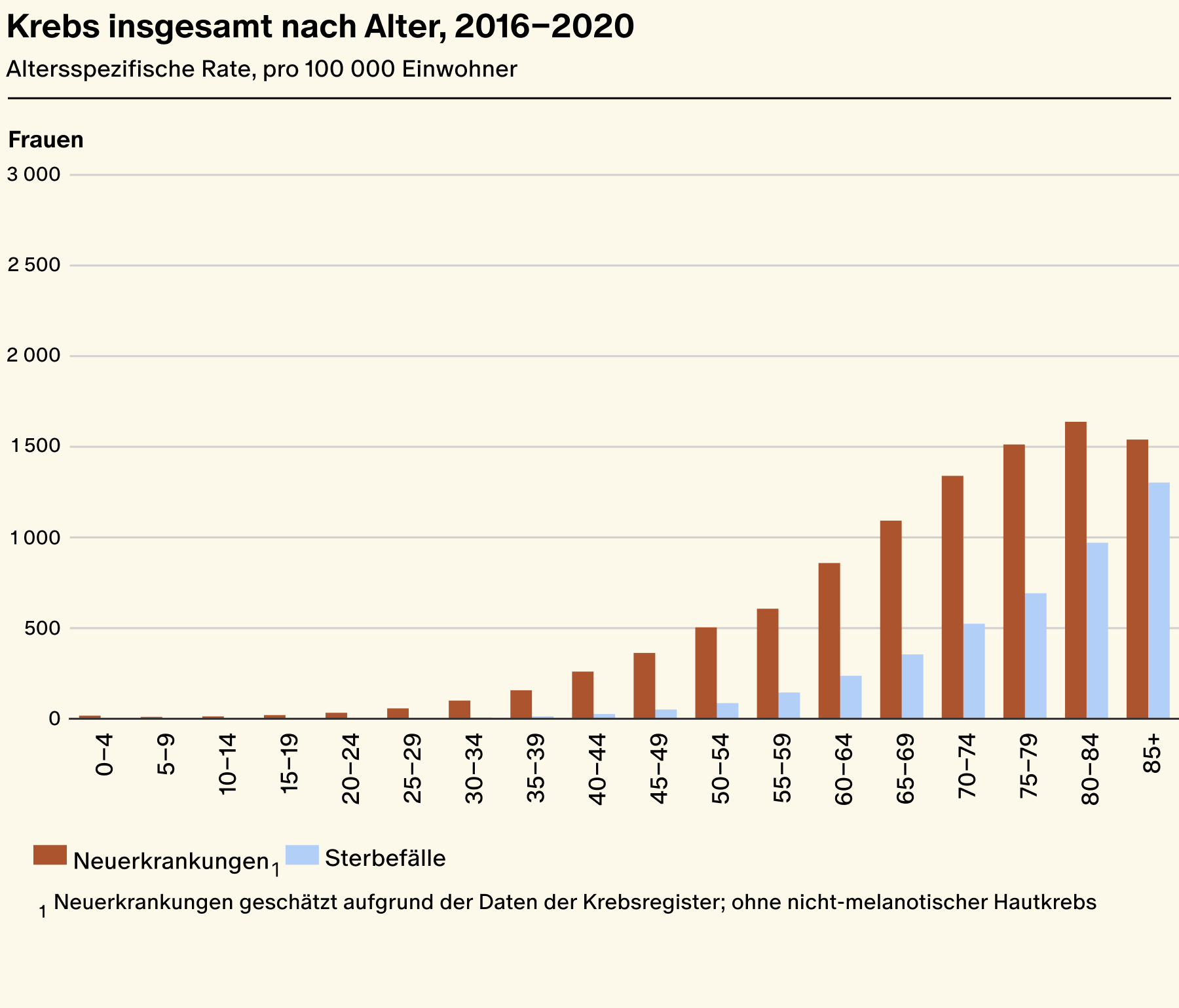
Over a four-year period (2016-2020), cancer incidence, i.e., the number of new cases per year in Switzerland, was 25,000 in men (55%) and 20,000 in women (45%). Thus, men are more likely to develop cancer than women.
According to the Cancer League, the four most common types of cancer in Switzerland are:
- Prostate cancer: The most common cancer in men, accounting for about 30% of all male cancer cases.
- Lung cancer: The second most common cancer in both men and women, accounting for about 11% of all new cases in men and 10% in women.
- Breast cancer: The most common cancer in women, making up 32% of all female cancer cases.
- Colorectal cancer: The second most common cancer in women, accounting for about 10% of all female cancer cases. In men, 10% of all cancers also affect the colon.
Relationship Between Age and Cancer Prevalence
The main risk factor for developing cancer is age. Most new cancer cases occur in older age, with the risk varying between men and women. The median age at first diagnosis for cancer patients is 66 years.
However, cancer prevalence changes with age. While children and adolescents are more often affected by leukemia or brain tumors, colorectal cancer, prostate cancer, and breast cancer are more common in adulthood.
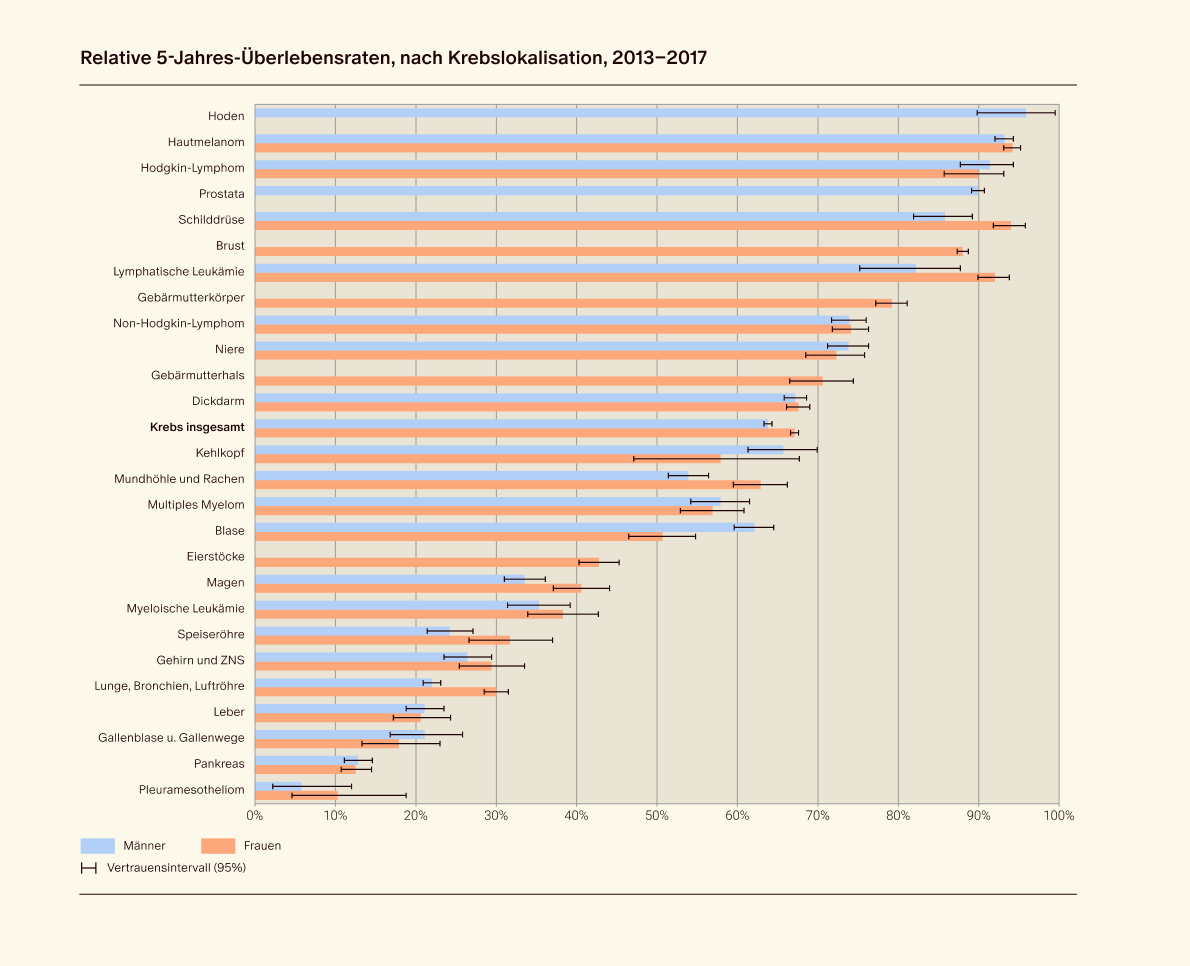
Significant Differences in Cancer Survival Rates
Survival chances after a cancer diagnosis vary greatly depending on the type of cancer. Testicular cancer, melanoma, Hodgkin lymphoma, prostate cancer, thyroid cancer, breast cancer, and lymphatic leukemia have the highest five-year survival rates, exceeding 80%.
In contrast, the five-year survival rate for patients with tumors of the pancreas, lung, gallbladder and bile ducts, and liver is below 30%.
The improved survival rates lead to a rising cancer prevalence, meaning that more and more people are living longer with the disease. Between 2006 and 2016, the number of cancer patients living for ten years or more after diagnosis increased from approximately 163,450 to around 210,350.
Highest Mortality Rate in Lung Cancer
Lung cancer, with 3,235 deaths per year, is the leading cause of cancer-related death for both men and women. This is despite the fact that lung cancer mortality has significantly decreased in recent years.
Most Common Cancer-Related Deaths:
Men:
- Lung cancer (21%)
- Prostate cancer (14%)
- Colorectal cancer (10%)
Women:
- Breast cancer (18%)
- Lung cancer (18%)
- Colorectal cancer (10%)
Decline in Mortality for Many Cancers
Over the past 30 years, age-standardized cancer mortality rates have decreased significantly:
- Men: -39%
- Women: -28%
This decline is observed across most types of cancer.
For prostate cancer, mortality decreased by 13% between 2013 and 2017.
There has also been a decline in mortality rates for breast cancer (-7%) and colorectal cancer (-13% in men, -7% in women) during the same period.
Increase in Mortality for Women
Early detection and advancements in cancer research generally contribute to lower death rates. However, in some cases, there has been an increase in cancer-related mortality among women:
- Slight increase in lung cancer mortality in women (+5%).
- Rising mortality rates in women for multiple myeloma, as well as liver and pancreatic cancers.
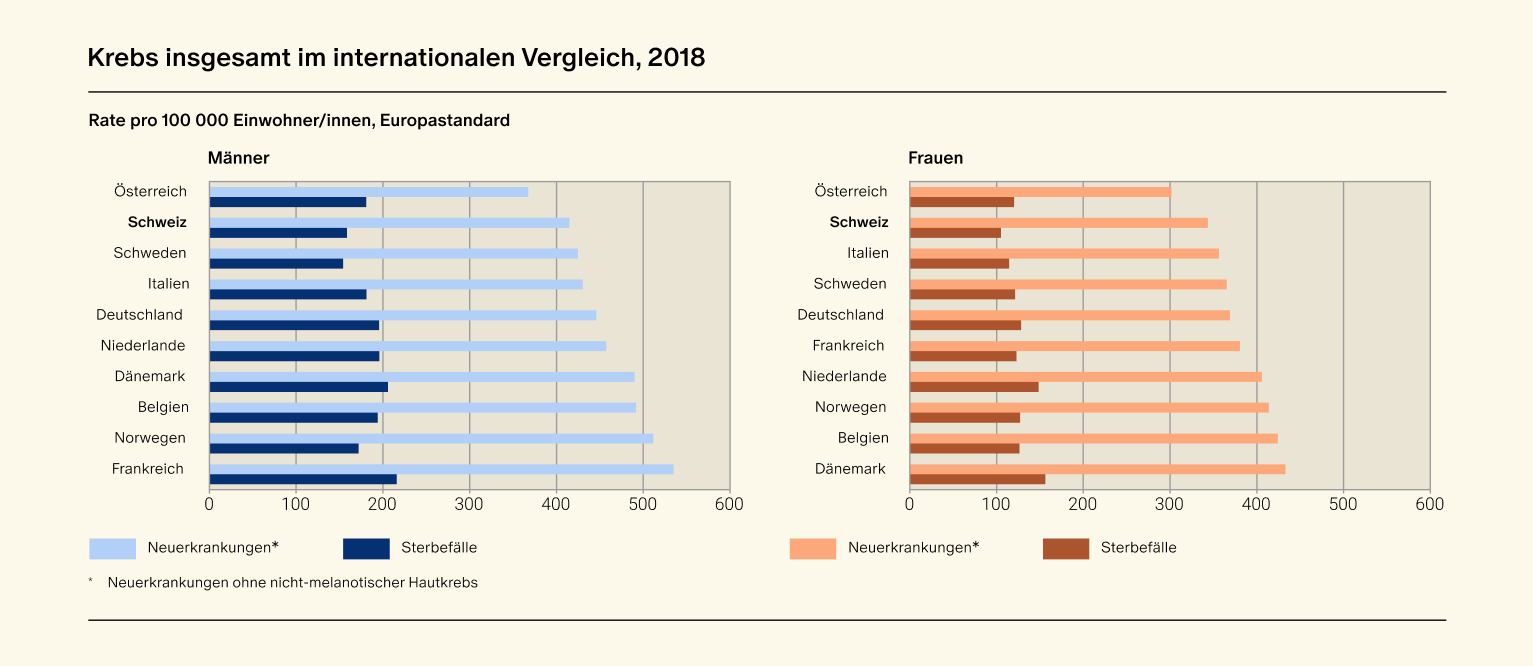
Good Survival Rates, Low Incidence and Mortality Rates
In a European comparison, Switzerland performs well in terms of cancer outcomes: Survival rates are average, while incidence and mortality rates are low.
Incidence:
- Men and Women: Compared to 9 other European countries, Switzerland has an overall low cancer incidence.
- Melanoma: An exception is melanoma, or skin cancer, which is the most dangerous form of skin cancer. Melanoma occurs above average in Switzerland, leading to a higher incidence rate.
Cancer Mortality:
- Women: In comparison to other countries, cancer mortality among women is low in Switzerland.
- Men: Six comparison countries have a lower mortality rate for men than Switzerland.
5-Year Survival Rate:
In terms of the 5-year survival rate, Switzerland ranks in the upper middle range.
Risk Factors for Cancer
The exact cause of cancer in individual cases is often difficult to determine. However, epidemiological studies show that various factors can contribute to the development of cancer. These factors can be divided into three main categories:
1. Behavioral Risk Factors:
- Smoking: Smoking is by far the most important risk factor for cancer. Tobacco smoke contains numerous carcinogens, which means it can cause cancer almost anywhere in the body. This includes cancers of the mouth, throat, esophagus, stomach, colon, rectum, liver, pancreas, larynx, lungs, trachea, bronchi, kidneys, renal pelvis, bladder, and cervix, as well as acute myeloid leukemia.
- Alcohol consumption: Excessive alcohol consumption can also increase the risk of various cancers, including liver, esophagus, colon, and breast cancer. The more alcohol a person regularly consumes over an extended period, the higher their risk of developing cancer. A French study found that in 2015, nearly 28,000 new cancer cases in France were due to alcohol consumption, accounting for 8% of new cancer cases.
- Unhealthy diet: A common myth is that red meat leads to cancer, but this is only partly true. It is often because people who eat a lot of (red) meat also tend to have an unhealthier diet. Furthermore, highly processed foods and beverages, due to their high sugar and sodium content, can lead to obesity and increase the risk of cancer.
- Lack of exercise: Physical inactivity is another risk factor for cancer. Regular exercise, on the other hand, can reduce the risk. The German Cancer Research Center refers to several studies showing that regular physical activity can lower the risk of cancer, especially colon cancer, with the protective effect being more pronounced in men than in women. Regular exercise can also reduce the risk of breast and uterine cancer (endometrial cancer). The relationship between exercise and lung cancer is not yet fully understood, and no clear link has been established between exercise and other types of cancer.
- Sun exposure: Excessive sun exposure without adequate protection can cause both non-melanoma and melanoma skin cancer. According to a report by the World Health Organization (WHO) and the International Labour Organization (ILO), sun exposure during outdoor work is a risk factor for non-melanoma skin cancer (NMSC). The study found that nearly one-third of deaths from this type of skin cancer are related to outdoor work.
2. External Environmental Risk Factors:
- Infections: Chronic infections with certain viruses and bacteria can increase the risk of various cancers. These include hepatitis B and C, Helicobacter pylori, and some types of human papillomavirus (HPV).
- Hazardous substances at work and in the environment: Exposure to certain hazardous substances at work or in the environment can increase cancer risk. These include asbestos, benzene, and radon.
- Air pollution: Air pollution can increase the risk of lung cancer. According to the WHO, 99% of the world's population is exposed to inadequate air quality. The health consequences of air pollution are similar to those of smoking, ranging from cancer to strokes and respiratory and cardiovascular diseases.
3. Individual Life History Factors:
- Genetic factors: Genetic predisposition to cancer can be inherited through a congenital mutation in the DNA. In 5 to 10% of cases, cancer occurs due to hereditary predisposition.
- Hormonal factors: Hormonal changes, such as early menarche, late menopause, or hormone replacement therapy, can increase the risk of certain cancers, such as breast and cervical cancer.
- Age: The older a person gets, the more likely they are to develop cancer. Age is actually the biggest risk factor for cancer, with more than nine out of ten cancers being diagnosed in people over 50 years old. People over 75 years of age make up about a third of all new cancer cases.
- Inflammation and autoimmune diseases: Over time, chronic inflammation can cause DNA damage and lead to cancer. People with chronic inflammatory bowel diseases, such as ulcerative colitis and Crohn's disease, have an increased risk of colorectal cancer.
- Medical treatments: Certain medical treatments, such as chemotherapy or radiation therapy, can increase the risk of secondary cancers.
Prevention: How to Reduce Cancer Risk
Cancer develops through a complex interaction of genetic and environmental factors. While genetic factors cannot be influenced, 30% of cancer cases in Switzerland can be prevented through preventive measures:
- Around 5% to 10% of all cancers are caused by inherited mutations in DNA.
- The remaining cancers arise due to carcinogens or an interaction between genetic predisposition and carcinogens.
- As a result, individual cancer risk can vary, even with the same exposure, depending on genetic susceptibility.
Prevention strategies:
- Avoiding risk factors like smoking, alcohol abuse, unhealthy diet, and lack of exercise
- Participating in vaccination programs (e.g., for HPV and hepatitis B)
- Engaging in screening programs (e.g., for breast and colorectal cancer), which can contribute to cancer prevention
In Switzerland, some cantons offer cancer screening programs focused on two of the most common types of cancer:
- Breast cancer: Early detection through mammography.
- Colorectal cancer: Early detection through a stool test and colonoscopy.
Recommendations for Cancer Prevention
The European Code Against Cancer and the World Health Organization (WHO) recommend the following measures to reduce cancer risk:
- Leading a healthy lifestyle
- Protecting against exposure to dangerous substances at work
- Getting vaccinated (HPV and hepatitis B)
- Regular participation in cancer screening
- Reducing radon exposure in indoor environments
- Promoting breastfeeding in women
- Limiting the use of hormone replacement therapies in women
- Avoiding unnecessary exposure to ionizing radiation (e.g., X-rays)
- Reducing indoor and outdoor air pollution levels






